User:Petergstrom/sandbox
Shortcuts
- Mechanisms of schizophrenia
- Biology of bipolar disorder
- Biology of depression
- Causes of mental disorders
- Cause of obsessive-compulsive disorder
- Biology of obsessive-compulsive disorder
Stats
GLM
| Distribution | Loglikelihood | Deviance | Valid Links | ||||
|---|---|---|---|---|---|---|---|
| Poisson | Id, ln, sqrt | ||||||
| Gaussian | Id, ln, power | ||||||
| Gamma | |||||||
| Bernoulli | |||||||
| Inverse Gaussian | |||||||
| Negative Binomial |
Factor Analysis
Factor analytic techniques in the most general form seek to model p observed variables as a linear combination of k usually latent or unobserved variables plus orthogonal error variance:
This can be formulated as the modeling of the observed sample covariance, denoted with the covariance implied by the factor analytic model . The model can be specified with a general class of fitting functions, the GLS functions of the general form for and which provided it provided V is a consistent estimator of the asymptotic covariance of the sample covariance(i.e. ), is asymptotically equivalent to estimation by maximum likelihood under normality assumptions, with the fitting function being
A common constraint, usually imposed under the name of Exploratory Factor Analysis(EFA), is The model without this constraint is usually called Confirmatory Factor Analysis(CFA)
Due to orthogonality constraints, EFA solutions are not unique, and is invariant under rotation by an orthogonal matrix. These rotations may be used to obtain a loadings matrices that has desirable properties for the given application(i.e. loadings forced towards zero or one).
Factor analysis is frequently confused with principal component analysis, but it differs as it is a probabilistic rather than a deterministic model, as PCA does not have an underlying generative model.
Fitting of the model by newton-raphson algorithms or MM algorithms(e.g. Expectation Maximization, or EMCM) usually require at least first order derivatives. These are, for a parameter vector
The inverse of the second matrix represents the observed fisher information matrix, , while the expected information can be expressed as
Popular methods of estimation include Lawley and Maxwell's maximum likelihood algorithm,[1] Rubin and Thayer's Expectation Maximization Algorithm[2], or generalized least squares.[3]
Pathophysiology of Depression
Neuroimaging
Structural Neuroimaging
- MDD > Ctrl : Ventricles, CSF
- Ctrl > MDD : Thalamus, hippocampus, frontal lobe, orbitofrontal gyrus, basal ganglia, gyrus rectus
- Current MDD <Remitted : Hippocampus
- WM/FA MDD<Ctrl : Frontal lobe, right fusiform gyrus, right occipital lobe
- ReHo MDD>Ctrl : mPFC
Functional Neuroimaging
- Altered patterns of activity were observed in the prefrontal and limbic regions, in support of the cortico-limib model
- Hyper-responsiveness in the amygdala, insula, and parahippocampal gyrus to negative facial stimuli
- Inconsistent magnitude of difference in the dlPFC, OFC and Cingulate gyrus, but a difference from control was consistently observed.
- Hypoconnectivity within the frontoparietal system, as well as between the frontoparietal system and the dorsal attention network.
- Hyperconnectivity within the default network.
- Depressed> Ctrl in response to negative stimuli, and Ctrl>Depressed in response to positive stimuli in Anterior Cingulate Cortex, Hippocampus, Amygdala, Striatum
- Altered activations of the striatum, insula, anterior cingulate in response to emotional stimuli.
- Hyperactivation in the anterior cingulate cortex, ventrolateral prefronta cortex, and hypoactivity in the caudate across all cognitive and emotional tasks
- Increased activity in the pulivnar nuclei, amygdala, insular, and anterior cingulate cortex in response to negative stimuli
- Decreased activity in the striatum in response to positive stimuli.
Molecular
Monoamines
- Reduced 5-HT1A receptor binding in the mesiotemporal cortex, the raphe nucleus, the insula and the anterior cingulate cortex.
- Reduced 5-HTT binding in the thalamus, amygdala, midbrain, striatum and brainstem.
- No altered striatal DAT availability
- 5-HT1A: Most literature points towards reduced BP in the mesiotemporal cortex, possible related with elevated cortisol
- 5-HT2A: PET examinations have found decreased BP, but post-mortem research suggests elevation in some depressed populations.
- 5-HTT: Moderate evidence for elevated 5-HTT activity in depression
- D1 receptor: Decreased in the striatum
- D2 receptor: Unclear
- Muscarinic Receptors: Evidence for elevation in depression
- The 5-HT/5-HIAA ratio, antidepressant efficacy gap, and failure of tryptophan depletion to elicit depression in health persons suggests elevated synaptic concentrations of serotonin in at least some subtypes of depression.
Inflammation
- Depression is associated with mild inflammation, and increased oxidative and nitrosative stress.
- Psychosocial stress is thought to contribute to depression by elevating inflammatory factors such as IL-1B, and TNF-alpha.
- These inflammatory factors alter processing in the anterior cingulate cortex, striatum, and cerebellum.
- Cytokines concentrations are elevated in depression, and trials with cytokine based treatments so far have been successful.
- A subset of depressed patients exhibit decreased cellular immunity, and elevated pro-inflammatory cytokines, which can alter neurotransmitter metabolis.
- The structural changes in the hippocampus and prefrontal cortex may be a result of chronic low grade inflammation, leading to altered kynurenine metabolism and the production of neurotoxic metabolites.
Genetics
- Shortened Telomere lengths in depression
- The heritability of depression is estimated at 31-42%.
- The BDNF Val66Met allele modulates the relationship between stress and depression
- The 5-HTT promotor region was associated with increased risk of depression, especially in association with stress and childhood maltreatment
- A meta analysis observed no significant SNPs, probably due to the complex and heterogenous nature of depression
- Significant SNPs included Metabotropic glutamate receptor 7 and ATP6V1B2
- No significant SNPs
Endocrine
- Dysregulated cortisol observed in the elderly with depression
- Increased cortisol but no increase in CRH
- https://www.ncbi.nlm.nih.gov/pubmed/20447770
- Increased morning and evening cortisol in depression
- https://www.ncbi.nlm.nih.gov/pubmed/15961250
- Depressed patients exhibited elavated recovery levels of cortisol after psychological stressors.
Neurogenesis
- Decreased peripheral measures of BDNF
- The decreased hippocampal volume appears in post mortem studies to be a result of altered neuroplasticity.
- Inflammatory factors in depression may lead to altered neuroplasticity through modulating neural stem cell survival, neurogenesis, dendritic branching and long term potentiation
- Decreased BDNF and decreased neuroplasticity in depression.
Antidepressants
- While antidepressants statistically significantly reduced hamilton depresson rating scale, this effect did not reach clinical significance, according to a predefined threshold set according to NICE standards. Overall, the risk outweighed the rewards.
- The monoaminergic activity of antidepressants correlated with long term risk of relapse, probably due to monoaminergic dys-homeostasis.
- The lack of a unified mechanism of antidepressants, and high placebo rates negate the small statistical difference between placebo and antidepressants. Supports the above studies finding that ADs may predispose to future relapse
- In adolescence and children, only fluoxetine was statistically more effective than placebo.
- Depression is effectively treated by TCAs and SSRIs, but most studies were of short duration and funded by pharmaceutical companies.
- Antidepressants are only better than placebo for patients with very severe depression(Hamilton>23)
- While antidepressants are statistically better than placebo, poor design quality and low effect sizes are characteristic of most studies.
- Moderate effect size for ADs, but over the years placebo efficacy has been increasing and response rates have been decreasing.
Pathophysiology of OCD
- Cortico-Basal Ganglia-Thalamocortical circuits
- Orbitofrontal cortex, anterior cingulate cortex
- Anxiety/Impulse control disorder
- Treated with
- CBT
- TCAs>SSRIs
Neuroimaging
Functional
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3079445/
- Functional neuroimaging studies usually report abnormalities in the OFC and ACC, although the direction is inconsistent
- https://www.ncbi.nlm.nih.gov/pubmed/15546704
- Meta analysis observed significant elevation of activity in the OFC and head of the caudate
- https://www.ncbi.nlm.nih.gov/pubmed/18787662
- During provocation of symptoms, significant activation likelihood was observed in the dorsolateral prefrontal cortex, precuneus, orbitofrontal cortex and ACC
- https://www.ncbi.nlm.nih.gov/pubmed/27276220
- OCD and ADHD share reduced ventromedial PFC GMV and functionality
Structural
- The left ACC and right OFC demonstrated decreased volume in OCD.
- Decreased FA observed in anterior midline tracts
- https://www.ncbi.nlm.nih.gov/pubmed/26733823
- OCD involve aberrant connectivity between the OFC and striatum
- https://www.ncbi.nlm.nih.gov/pubmed/20603451
- OCD demonstrates increased bilateral lenticular and caudate volumes relative to other anxiety disorders
Structural/Functional Reviews
- Affective dysfunction appears to underly and link obsessions and compulsions.
- Amygdala hyperactivity in response to fearful stimuli, and, along with the ventral striatum, hypoactivity in response to positive stimuli.
- Structural and functional imaging suggests the involvement of the OFC-Striatal circuit, which involved the OFC/ACC, and basolateral amygdala/hippocampus projecting to the ventral striatum, which in turn projects to the globus padillus and returns to the OFC/ACC/amygdala/hippocampus through the thalamus.
- Structural alterations were observed in the cerebellar, frontal, striatal and thalamic regions, implicating dysfunction of the corticobasal ganglia thalamocortical loop in OCD. Furthermore, deficits in functionality localized to these regions such as inference, inhibition and task switching were observed.
- OCD appears to have five different subtypes, of which the hoarding subtype appears to have a different underlying neurobiological mechanism
- The altered corticolimbic circuitry likely results in an excessive reliance in habit based learning and deficits in goal directed behavior
- OCD and ADHD demonstrate similar deficits in executive function, and involve dysfunction in overlaping corticostriatal circuits
- https://www.ncbi.nlm.nih.gov/pubmed/22678698
- There is a significant association altered functionality cortico-basal ganglia-thalamocortical circuits and OCD, despite inconsistencies in the direction of changes
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4476073/
- Theoretical SEC model suggests that various behavioral patterns represented in the cortex are executed with the help of motivational signals.
- In OCD, the ACC generates aberrant SEC error signals, and anxiety arises from limbic systems. The basal ganglia then generates "compensatory" SECs in the form of compulsions.
- OCD models defined by two neuropsychological facets, executive function and modulatory control. The first model involves dysfunction in the dlPFC, striatum, and thalamus, and the second of which involves dysfunction in the OFC and ACC
- OCD involves inflexibility of internal cognition, and supporting this notion is the observation of altered DMN activity
Genetic
- The 5-HTTPR S type was associated with OCD, but only in females
- Moderate association between OCD and SNPs of the glutamate transporter
- OCD was associated with 5-HTTPLR and 5-HT2A gene polymorphisms, and in males only, the COMT and MAO-A genes
- OCD was associated with https://www.ncbi.nlm.nih.gov/gene/79154, https://www.ncbi.nlm.nih.gov/gene/140862, and DLGAP1
- While no overall association between the 5-HTTPLR S or L gene with OCD, family based studies found an association between the L type and OCD in caucasians
- Microstructure abnormalities were observed in the ACC and OFC pathways to the basal ganglia, and hyperconnectivity in the genu of the corpus callosum.
- Association between OCD and COMT polymoprhism, but only in men.
- No association between COMT and OCD
- OCD was associated with 5-HTTPLR SS allele, but inversely with the LS allele
Neurochemical
- 5-Fold increase in risk of anti-basal ganglia antibodies in OCD, supporting the theory that a subset of OCD involve basal ganglia auto-immunity
- Reduced N-Acetylaspartate in the medial PFC in OCD
- While some evidence suggests "elevated" dopamine in OCD, however this is contradicted by much evidence, including the fact that antipsychotics can exacerbate OCD, and the observation of contradictory molecular imaging findings with regard to DAT
- Elevated CSF glutamate
- Inconsistent molecular imaging studies about glutamate, although abnormalities have been frequently observed
- Significant association between glutamate regulating genes and OCD
Dopaminergic Modulation of the PFC
- Phasic dopamine release in the prefrontal cortex is capable of mediating cognitive flexibility. Activation of D1 receptors on a neuron increases the influence of strong signals and inhibits the weaker signals, effectively strengthening the representation of information in the PFC. D2 receptors on the other hand increase sensitivity to external noise, resulting in increased cognitive flexibility. This dynamic enables a switch in focus due to a salient stimulus. Given that D2 receptors tend to be synaptic, and D1 receptors tend to be extrasynaptic, phasic transmission is characterized first by preferential D2 activation, followed by tonic D1 activation. A salient stimulis can then trigger a transition state, followed by restrengthening.[4]
- The role of DA in modulating the PFC is conceptualized by two regimes. The D1 dominated regime is characterized by a "robust", "high energy barrier" that facilitates the maintenance of information. The D2 dominated regime is in turn characterized by a low energy barrier that facilitates quick transition between representational states.[5]
Bipolar Disorder
Etiology
The etiology of bipolar disorder is unknown. The overall heritability of bipolar is estimated at 79%-93%, and first degree relatives of bipolar probands have a relative risk of developing bipolar around 7-10. While the heritability is high, no specific genes have been conclusively associated with bipolar, and a number of hypothesis have been posited to explain this fact. The polygenic common rare variant hypothesis suggests that a large number of risk conferring genes are carried in a population, and that a disease manifests when a person has a sufficient number of these genes. The multiple rare variant model suggests that multiple genes that are rare in the population are capable of causing a disease, and that carrying one or a few can lead to disease.
A number of genome wide associations have been reported, including CACNA1C and ODZ4. Less consistently reported loci include ANK3 and NCAN, ITIH1, ITIH3 and NEK4. Significant overlaps with schizophrenia have been reported at CACNA1C, ITIH, ANK3, and ZNF804A. This overlap is congruent with the observation that relatives of probands with schizophrenia are at higher risk for bipolar disorder and vice versa. In light of associations between bipolar and circadian abnormalities(such as decreased need for sleep and increased sleep latency), polymorphisms in the CLOCK gene have been tested for association, although findings have been inconsistent.[6] Other circadian genes associated with bipolar at relaxed significance thresholds include ARTNL, RORB, and DEC1.[7]
Pathophysiology
Structural neuroimaging studies consistently report increased frequency of white matter hyperintensities in people with bipolar. However, whether or not the lesions play a causative role is unknown. It is possible that they are a result of secondary factors, such as in increased risk of cardiovascular disease in bipolar. On the other hand, the observation of reduced white matter integrity in frontal-subcortical regions makes it possible that these hyperintensities play a role dysfunction between limbic and cortical regions. Global brain volume and morphology are normal in bipolar. Regional deficits in volume have been reported in ventrolateral and dorsolateral prefrontal regions. Based on this, it has been suggested that reduced limbic regulation by prefrontal regions plays a role in bipolar. Findings related to the volume of the basal ganglia have been inconsistent.
Functional neuroimaging studies, contrary to structural studies, consistently find hyperactivation of the basal ganglia, amygdala, and thalamus. Prefrontal abnormalities are less consistently reported, although hyperactivation in the ventral prefrontal cortex is a fairly consistent finding.[8] Mania is generally associated with frontal/ventral hypoactivation, while depression is generally associated with the opposite. A degree of lateralization with regard to abnormalities has been reported, with mania being associated with the right hemisphere, and depression the left. Trait abnormalities in euthymic patients have been observed, including hypoactivity in the ventral prefrontal cortex, and hyperactvity in the amygdala.[9]
Cause
- Juvenile onset; Mood lability.
- Are there different genotypes in Bipolar II and Bipolar I disorder and if so, why then do we tend to observe Unipolar Depression converting to Bipolar II and then converting to Bipolar I?
- Predicting bipolar disorder on the basis of phenomenology: implications for prevention and early intervention.
- COMT/DRD3/DRD2/BDNF polymorphisms distinguish BPI from BPII
- Interactions Between Variation in Candidate Genes and Environmental Factors in the Etiology of Schizophrenia and Bipolar Disorder: a Systematic Review.
- Epidemiological and clinical variables related with the predominant polarity on bipolar disorder: A systematic review.
- Predominately manic BP==pre onset drug use and earlier dx
Genetics
- Exome Sequencing of Familial Bipolar Disorder.
- A survey of genomic studies supports association of circadian clock genes with bipolar disorder spectrum illnesses and lithium response.
- ARTNL, RORB, and DEC1 all associated with BP
- Association at SYNE1 in both bipolar disorder and recurrent major depression.
- Meta-analysis confirms a functional polymorphism (5-HTTLPR) in the serotonin transporter gene conferring risk of bipolar disorder in European populations.
- TPH2 gene polymorphisms and bipolar disorder: A meta-analysis.
- Association between brain-derived neurotrophic factor genetic polymorphism Val66Met and susceptibility to bipolar disorder: a meta-analysis.
- Genetics of bipolar disorder.
- Comparative Linkage Meta-Analysis Reveals Regionally-Distinct, Disparate Genetic Architectures: Application to Bipolar Disorder and Schizophrenia
- Meta-analysis of genetic association studies on bipolar disorder.
- The Genetics of Bipolar Disorder
- Meta-analysis of genome-wide association data of bipolar disorder and major depressive disorder
- Genomic View of Bipolar Disorder Revealed by Whole Genome Sequencing in a Genetic Isolate
- Genetics of bipolar disorder
Environmental
- Gene environment interactions in bipolar disorder.
- Beyond genetics: childhood affective trauma in bipolar disorder.
- A Review of Bipolar Disorder in Adults
- Prenatal Programming of Mental Illness: Current Understanding of Relationship and Mechanisms
- A theoretical framework informing research about the role of stress in the pathophysiology of bipolar disorder.
- The HPA axis in bipolar disorder: Systematic review and meta-analysis.
- Predominately manic BO associated with drug use and earlier diagnosis
Mechanism
- Variation in CLOCK genes and circadian rhythm associated with BPD
- Season variation in BPD symptoms, with manic switches occurring during long photoperiods and depression episodes occurring during periods with less light. Furthermore, photoperiod induced variations in tyrosine hydroxylase expression support a role of catecholamine dysregulation in BPD.
- Inconsistent evidence across D2 type receptors and DAT in both post-mortem studies but D1Rs BP is decreased/prbly due to increase synaptic conc
- Pharmacological models of mania are generally DA release agents, and mood stabilizers reduce DA synthesis and release
- Reduced in vivo BP of muscarinic receptors in BPD Dep, and decreased receptor expression in post-mortem studies-likely due to excessive synaptic conc
- Pharmacological support^^
- Decreased vlPFC activity in both euthymic and manic bipolar disorder
- Decreased activity(likely indicative of increased DA stimulation) in the striatum in mania, and increased activity in euthymia
- Elavated dorsal ACC activity in mania
- Thinning of the vmPFC and well as enlargement of ventricles correlates with manic episodes
- More cells in the LC, slightly fewer cells in the RN
- Hyperresponsiveness of the HPA axis correlated with longer duration of affective episodes
- Delayed sleep phase in common in BPD, sleep efficiency is decreased, higher density of REM sleep
- Nighttime correlates with symptom presentation, exaggerated melatonin reduction in response to light, and elevated afternoon cortisol.
- Most anti-manic drugs alter intracellular GSK-3 signaling.
- The underlying neurobiology of bipolar disorder
- The Psychopathology and Treatment of Bipolar Disorder
- Contributions from brain imaging to the elucidation of pathophysiology of bipolar disorder
- New insights help define the pathophysiology of bipolar affective disorder: neuroimaging and neuropathology findings
Neurocircuits
- A critical appraisal of neuroimaging studies of bipolar disorder: toward a new conceptualization of underlying neural circuitry and a road map for future research.
- Dysfunction in emotional regulatory circuits characterized by reduced prefrontal-amygdala connectivity
- Hypersensitivity to reward indicated by elevated ventral striatal, ventrolateral prefrontal, and orbitofrontal cortex response to positive emotional stimuli.
- The functional neuroanatomy of bipolar disorder: a consensus model
- Structural neuroimaging studies in the early stages of bipolar suggests that the progressive nature of bipolar disorder reflects dysregulated growth and connectivity in prefrontal-limbic circuits, especially in the amygdala
- Neural circuits underlying the pathophysiology of mood disorders
- Functional neuroanatomy of bipolar disorder: structure, function, and connectivity in an amygdala-anterior paralimbic neural system
- Elevated reward-related neural activation as a unique biological marker of bipolar disorder: assessment and treatment implications/
- Corticolimbic connectivity as a possible biomarker for bipolar disorder
- Overlapping prefrontal systems involved in cognitive and emotional processing in euthymic bipolar disorder and following sleep deprivation: a review of functional neuroimaging studies
- Brain network dysfunction in bipolar disorder.
Neurobiological
- Dysregulation of the NF-κB pathway as a potential inducer of bipolar disorder.
- Developmental meta-analyses of the functional neural correlates of bipolar disorder.
- Could glutamate spectroscopy differentiate bipolar depression from unipolar?
- Functional neuroanatomy of response inhibition in bipolar disorders--combined voxel based and cognitive performance meta-analysis.
- Neurometabolites in schizophrenia and bipolar disorder - a systematic review and meta-analysis.
- A systematic review and meta-analysis of proton magnetic resonance spectroscopy and mismatch negativity in bipolar disorder.
- Evidence of diagnostic specificity in the neural correlates of facial affect processing in bipolar disorder and schizophrenia: a meta-analysis of functional imaging studies.
- Brain glutamate levels measured by magnetic resonance spectroscopy in patients with bipolar disorder: a meta-analysis.
- Circadian abnormalities as markers of susceptibility in bipolar disorders.
- Origin of cyclicity in bipolar disorders: a computational approach.
- Neurophysiological findings in patients with bipolar disorder.
- Translating neurotrophic and cellular plasticity: from pathophysiology to improved therapeutics for bipolar disorder.
- Calcium signalling and psychiatric disease: bipolar disorder and schizophrenia.
- Role of neuro-immunological factors in the pathophysiology of mood disorders.
- Neurotrophins, inflammation and oxidative stress as illness activity biomarkers in bipolar disorder
- Signaling: cellular insights into the pathophysiology of bipolar disorder.
- The possible involvement of NMDA glutamate receptor in the etiopathogenesis of bipolar disorder.
- Investigating the underlying mechanisms of aberrant behaviors in bipolar disorder from patients to models: Rodent and human studies.
- Molecular neurobiological clues to the pathogenesis of bipolar disorder.
- Metabotropic glutamate receptors as emerging research targets in bipolar disorder.
- Brain structure, function, and neurochemistry in schizophrenia and bipolar disorder-a systematic review of the magnetic resonance neuroimaging literature.
- Gray matter abnormalities as brain structural vulnerability factors for bipolar disorder: A review of neuroimaging studies of individuals at high genetic risk for bipolar disorder.
- The structural neuroimaging of bipolar disorder.
- Magnetic resonance findings in bipolar disorder.
- Functional neuroimaging studies of bipolar disorder: examining the wide clinical spectrum in the search for disease endophenotypes.
- Wnt and GSK3 Signaling Pathways in Bipolar Disorder: Clinical and Therapeutic Implications.
- Neurobiology of Risk for Bipolar Disorder.
- Dissecting bipolar disorder complexity through epigenomic approach.
- Mania secondary to focal brain lesions: implications for understanding the functional neuroanatomy of bipolar disorder.
- The Neurobiology of Bipolar Disorder: An Integrated Approach.
- The Neurobiology of Bipolar Disorder: An Integrated Approach.
- The relationship between genetic risk variants with brain structure and function in bipolar disorder: A systematic review of genetic-neuroimaging studies.
- The relationship between bipolar disorder and biological rhythms.
- The neuropsychology and neuroanatomy of bipolar affective disorder: a critical review.
- The relationship between genetic risk variants with brain structure and function in bipolar disorder: A systematic review of genetic-neuroimaging studies.
- The dopamine hypothesis of bipolar affective disorder: the state of the art and implications for treatment.
- Neurobiological underpinnings of bipolar disorder focusing on findings of diffusion tensor imaging: a systematic review.
- Can neuroimaging disentangle bipolar disorder?
GSK-3
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3055312/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4523227/
- http://journal.frontiersin.org/article/10.3389/fnmol.2012.00001/full
IP
Psychosis
Models
- Risk factors: toxoplasmosis gondii, Obstetric complications, Low birth weight, Urban environment,Immigration Status,Childhood trauma
- Neurexin SNPs associated with schizophrenia
- Drawn out period of development, remodeling and instability lasts into late thirties
- Reduced mRNA of GAD67 in the PFC, reduced GABAergic cells, reduced inhibitory synapses
- Prenatal stress increases risk of schizophrenia, and has been demonstrated to lead to delayed migration, and morphological changes in PFC cells.
- Reelin has been demonstrated to be hypermethylated in schizophrenia, and therefore under expressed. Heterozygous knockout mouse demonstrate similar alterations in neurodevelopment, and a reduction in GABAergic neurons that are characteristic of schizophrenia. Furthermore, stress had been observed in animal models to lead to underexpression
- Functional neuroimaging studies have found that aberrant prediction error signalling occurs in schizophrenics, and correlates with delusion severity
- Schizophrenics are more susceptible to illusions produced by altering sensory experience
- Schizophrenics demonstrate abnormalities with predicting the effects of their actions
- The role of NMDA in schizophrenia and the ability for NMDA anagonists to mimic schizophrenia fit in with the model suggesting that delusions are a result of dysfunctional prediction systems
- Morphological differences in dendrites
- Schizophrenics demonstrate deficits in the ability to correctly attribute stimuli, or link actions to sensory outcomes. Disruption of the thalamocortical gamma bands may play a role.
- Abnormal connectivity between the frontal and parietal lobes are suggested to give rise to a decreased sense of control, but an increased sense of agency
Cause
Genetics
- Genes associated with SCZ include TCF4, NRGN, VRK2, MIR137, PCGEM1, CSMD1, MMP16, CNNM2, NT5C2, and CACNA1C
- The most commonly associated genes are generally involved in MHC regions, synaptic plasticity, and neurodevelopment
- DGCR8 has been observed to be prone to deletion in schizophrenics, and is deferentially expressed.
- DGCR8 being differential expressed leads to altered transcription of synaptic proteins.
- Increased methylation of H3 histone R17 in the PFC of schizophrenics
- Most neuroimaging studies demonstrate a more significant effect size compared to cognitive studies. The greatest gene associated with neuroimaging alterations was DAOA
- Most of the genes associated with recent primate evolution that are associated with schizophrenia are involved in synaptic regulation, and are expressed in the PFC in higher concentrations.
- Genetic influences on schizophrenia and subcortical brain volumes: large-scale proof of concept.
- Evaluating historical candidate genes for schizophrenia
- No historical candidate genes were found to be significant in the SZgene study, but four genes (DRD2, GRM3, NOTCH4, TNF) have been found to be significant in the PCG. Two have been found in the MHC.
- NRXN1 and MHC genes have been most frequently associated with schizophrenia(along with NOTCH4 and the aforementioned TNF)
Environment
- Infections during the prenatal period have been associated with schizophrenia. Some evidence points towards the effect of pro-inflammatory proteins on neurodevelopment(including IL-8 and TNF)
- Famine and materna nutritional deficiencies have been associated with an increase risk of schizophrenia.
- Advanced paternal age
- Prenatal stress has been linked to schizophrenia, but not as strongly as low birth weight, which prenatal stress has been strongly linked with. CRH and inflammatory mechanisms may be involved
- Cannabis use has been associated with schizophrenia when used in adolescence, and a dose response relationship has been suggested. This finding has been replicated a number of times, with a meta analysis reporting a pooled odds ratio of 2.3 in studies assessing cannabis use before schizophrenia onset, suggesting a causative role.
- While most genetic and environmental studies have reported small effects, assessing GxE associations has significantly increased effect.
- Urbanization, childhood stress, migration, and adverse life events, and being born during the winter or spring have been associated with schizophrenia.
- Oxidative stress may cause NMDA receptor hypofunction due to genetic alterations in synaptic regulation combined with stress.
- Along with the aforementioned associations with infections and maternal famine, maternal obesity has been associated with SCZ as well.
Mechanism
Neurochemical
- Post mortem studies while few in number are associated with a reduction in post-synaptic dopamine receptors, and an increase in presynaptic D2 receptors, as well as an increase in TH, no change in DAT, elavation of D4 receptors, a reduction in D2 monomers, and a large increase in D2 dimers
- In Vivo neurochemical imaging has demonstrated a large increase in presynaptic dopamine metabolism, but the post-synaptic dopaminergic protein results have been inconsistent
- While genetic studies and the mimicry of SCZ symptoms by NMDA agonists implicates glutamate dysfunction in SCZ, a lack of consistency in post-mortem studies suggests that a deficit in NMDA receptor expression may be too simple a model, rather NMDA dysfunction may be characterized by dysfunctional regional expression and altered subunit composition.
- While those with familial risk, first episode psychosis, or psychotic symptoms demonstrate increased glutamine levels using in vivo imaging, chronic schizophrenics demonstrate a reduction or normal levels. Furthermore, an increase in glutamine/gluamate ratio has been observed in some studies
- Due to the lack of a definitive neurodegenerative course in the morphological changes associated with schizophrenia, the common finding of reduced cortical thickness and increase ventricle volume are thought to be a result of developmental processes.
- Variable findings in interstitial white matter have been observed with regard to GABAergic neurons.
- Both genetic and environmental risk factors for SCZ have been associated with altered GABAergic development
- Significant elavation in presynaptic dopamine metabolism, increase in D2/D3 receptor expression(post-synaptic) and no effect on DAT
- Altered expression of D1 in the ACC, uncus, and D2 in the PFC have been osberved, as well as DAT alterations in the thalamus
- D2 receptor expression in the thalamus and ACC is reduced in schizophrenia
- Stimulant evoked DA release is elevated in the striatum, but reduced elsewhere
Neurobiological
- NMDARs are necessary for large network connectivity and heavily influence GABAergic development. Both genetic and post-mortem studies have demonstrated alterations in GABAergic and NMDAR proteins and regulating genes, and a widely replciated finding is a reduction in NMDA receptors globally, although this effect is particularly significant in GABAergic neurons, and is especially prominent in NR1 and NR2C subunits in the PFC.
- Intact GABAergic signalling is necessary for gamma band activity
- Younger SCZs demonstrate decreased expression of PSD-95 with concurrent increases in thalamic NR2B, while the elderly with SCZ demonstrate the inverse.
- Expression of NMDA subunits appears to be decreased in the prefrontal cortex, as well as in general. Combined with evidence from NMDA receptor antagonists, this data suggests that schizophrenia involves hypofunctioning of NMDA receptors. This may contribute to resting state abnormalities in connectivity, as well as dopaminergic abnormalities.
Neurocircuitry
- Ehh not really a great review
- Paywalled
- Ctrl>SCZ: dlPFC, Amygdala, Hippocampus, ACC, Thalamus, Caudate and Midbrain.
- SCZ>Ctrl: Parietal Lobule, Precentral Gyrus and STG.
- Variable Amygdala findings, possibly reflecting general reduced responsively to social stimuli.
- Detecting neuroimaging biomarkers for schizophrenia: a meta-analysis of multivariate pattern recognition studies.
- Meta-analysis of 41 Functional Neuroimaging Studies of Executive Function in Schizophrenia
- Ctrl>SCZ: dlPFC, right vPFC, rACC and anterior ACC extending into the mPFC, right ventral PMC, putamen and thalamus.
- SCZ>Ctrl: left dorsal and ventral PMC, dorsal ACC and amygdala.
- Possible due to frontal top down dysfunction, leading to brain wide dysfunction
- Although reduced dlPFC was observed, hyperactivity in the frontal pole and ACC were also found
- Ctrl>SCZ bilaterally in the IFG and SMA, and unilaterally in the basal ganglia, superior OCC, SMA, IPG, and cuneus.
- SCZ>Ctrl in post-central gyrus and fusiform gyrus
- Reduction in STG over course of SCZ
- Reductions in GMV were seen in the insula and ACC,the left parahippocampus, left MFG, left postcentral gyrus, and left thalamus.
- Subcortical brain volume abnormalities in 2028 individuals with schizophrenia and 2540 healthy controls via the ENIGMA consortium.
- Reduced hippocampus, amygdala, thalamus, NAcc, and GP volumes.
- Structural correlates of auditory hallucinations in schizophrenia: a meta-analysis.
- AVH correlated with Ctrl>SCZ in left ins, right STG
- Ctrl>SCZ: FA/WM in inter hemispheric fibers, anterior thalamic radiations, inferior longitudinal occipital fascicule, cingulum, and fornix
- Ctrl>SCZ: GM in Insula, Interior frontal cortex, STG, ACC, thalamus, left amygdala
BG
- Selection of actions in the basal ganglia-thalamocortical circuits: review and model.
- Synaptic organisation of the basal ganglia
- Chapter 6 Basal ganglia-thalamocortical circuits: Parallel substrates for motor, oculomotor, “prefrontal” and “limbic” functions
- Functional anatomy of the basal ganglia. I. The cortico-basal ganglia-thalamo-cortical loop.
- Functional architecture of basal ganglia circuits: neural substrates of parallel processing.
- The primate basal ganglia: parallel and integrative networks.
- Changing Views of Basal Ganglia Circuits and Circuit Disorders
- Update on models of basal ganglia function and dysfunction
- The cortico-basal ganglia integrative network: the role of the thalamus
- Circuits and Circuit Disorders of the Basal Ganglia
- Thalamic Relay Nuclei of the Basal Ganglia Form Both Reciprocal and Nonreciprocal Cortical Connections, Linking Multiple Frontal Cortical Areas
- The cortico-basal ganglia-thalamocortical circuit with synaptic plasticity. II. Mechanism of synergistic modulation of thalamic activity via the direct and indirect pathways through the basal ganglia
- Basal ganglia and cerebellar loops: motor and cognitive circuits
- PARALLEL ORGANIZATION OF FUNCTIONALLY SEGREGATED CIRCUITS LINKING BASAL GANGLIA AND CORTEX
- FROM REINFORCEMENT LEARNING MODELS OF THE BASAL GANGLIA TO THE PATHOPHYSIOLOGY OF PSYCHIATRIC AND NEUROLOGICAL DISORDERS
- The basal ganglia: An overview of circuits and function
- Parallel basal ganglia circuits for voluntary and automatic behaviour to reach rewards
- Basal ganglia circuit loops, dopamine and motivation: A review and enquiry
- The basal ganglia: a vertebrate solution to the selection problem?
- Computational models of basal-ganglia pathway functions: focus on functional neuroanatomy
- Direct and Indirect Pathways of Basal Ganglia: A Critical Reappraisal
- Integration of Navigation and Action Selection Functionalities in a Computational Model of Cortico-Basal-Ganglia–Thalami-Cortical Loops
- Inhibitory Control in the Cortico-Basal Ganglia-Thalamocortical Loop: Complex Regulation and Interplay with Memory and Decision Processes
- Functional Neuroanatomy of the Basal Ganglia
- Physiology and pathophysiology of the basal ganglia-thalamo-cortical networks.
- Physiology and pathophysiology of cortico-basal ganglia-thalamocortical loops: theoretical and practical aspects.
- Basal ganglia-thalamocortical circuits: their role in control of movements.
- Inhibitory Control in the Cortico-Basal Ganglia-Thalamocortical Loop: Complex Regulation and Interplay with Memory and Decision Processes
- Neuronal circuits and physiological roles of the basal ganglia in terms of transmitters, receptors and related disorders.
- Basal ganglia circuit loops, dopamine and motivation: A review and enquiry.
- Striatal direct and indirect pathways control decision-making behavior.
- Functional implications of dopamine D1 vs. D2 receptors: A 'prepare and select' model of the striatal direct vs. indirect pathways.
- Reassessing models of basal ganglia function and dysfunction.
- The place of dopamine in the cortico-basal ganglia circuit.
- The basal ganglia, the ideal machinery for the cost-benefit analysis of action plans.
- Goal-directed and habitual control in the basal ganglia: implications for Parkinson's disease.
- Cholinergic interneurons in the dorsal and ventral striatum: anatomical and functional considerations in normal and diseased conditions.
- Investigating striatal function through cell-type-specific manipulations.
- Striatal plasticity and basal ganglia circuit function.
- Contributions of the striatum to learning, motivation, and performance: an associative account.
- Corticostriatal circuitry.
- Cortico-basal ganglia networks subserving goal-directed behavior mediated by conditional visuo-goal association.
Schizophrenia cont
- The symptoms of schizophrenia largely fall into three categories, reality distortion, negative symptoms and disorganization. The dichotomy, traced back to work by Kraepalin, whereby bipolar affective and psychotic disorders are treated as separate entities, is contradicted by continuity of affective and psychotic symptoms through genetic and neurobiological factors.[10]
- The heritability of Schizophrenia is estimated to be roughly 80%. The heritable component is evident in monozygotic and dizygotic concordance, 41-65% and 0-28% respectively, as well as the elevated risk of developing in schizophrenia in those with first degree relative with schizophrenia, or bipolar disorder. Schizophrenia has been associated in GWAS studies with.[11]
- MIR137
- SDCCAG8-rs6703335
- VRK2-rs2312147
- ZNF804A-rs1344706
- PCGEM1-rs17662626
- ITIH3-rs2239547
- Extended Major Histocompatibility Complex Regions
- CSMD1-rs10503253
- LSM1-rs16887244
- MMP16-rs7004633
- ANK3-rs10994359
- CNNM2-rs7914558
- NT5C2-rs11191580
- AMBRA1-rs11819869
- ODZ4-rs12576775
- NRGN-rs12807809
- CACNA1C-rs4765905
- TCF4-rs9960767
- CCDC68-rs12966547
- NCAN-rs1064395
Significant overlap in GWAS studies of bipolar and schizophrenia have been observed at ANK3, CACNA1C, ZNF804A, and ITIH3-ITIH4. Studies of brain structure and function in Schizophrenia have included longitudinal, patient-control constrast, and at-risk study designs. Schizophrenia is associated with reduced volumes, usually of the magnitude 5-10%. Robust structural findings include 1)Ventricular enlargement, 2)Reduced whole brain volume, 3)Reduced GMV of the medial temporal lobe extending to the hippocampus and amygdala, 4)Reduced GMV in the STG. thirty-five out of forty-six studies report significant STG volume reduction, and eighteen out of thirty studies reported correlations between STG volume and severity of auditory hallucinations or though disorders. Thirteen studies have reported bilateral thalamic reductions, including studies on both first episodes and chronic patients. Grey matter reductions are particularly evident in the anterior ingulate, medial and inferior frontal lobes, and anterior insula. Bipolar parients and Schizophrenic pateints exhibit significant overlaps in the ACC, mPFC, lPFC, and bilateral insula, only differing in magnitude. The Cerebellum, Corpus Callosum, and Basal Ganglia are frequently observed to be structurally abnormal, although the findings as well as direction of changes is inconsistent. Longitudinal neuroimaging suggests that schizophrenia appears to be more of a neurodevelopment disorder, rather than a neurodegenerative disorder.[12] Schizophrenics exhibit hypoactivity in the dlPFC during executive function tasks, frequently extending to the ACC, thalamus, and inferior and posterior parietal cortices. Hyperactivity during executive function tasks have been observed in midline cortical regions, premotor cortcices and the vlPFC. Reduced activation of the dlPFC during episodic memory tasks has been observed. Reality distortion has been assocaited with increased medial temporal blood flow, and decreased prefrontl boodflow in the other two symptom dimensions. Negtative symptoms in schizophrenia are characterized by more pronounced and widespread GMV losses. MTL generally differentiates affective disorders from less affective psychotic disorders. Longitutinally, Schizophrenia is associated with continual reductions in thalamic and prefrontal volumes and less consistend temporal lobe changes. Hippocampal reductions over time are more contested. In those at high risk for psychosis, inferior frontal and superior temporal reductions are associated with transition to psychosis. Magnetic resonance spectroscopy observe first episode increased in Gln and decreased in Glu, followed by accelerated age related decreased in Gln and Glu relative to controls--->Taken to mean first episode increased in Glu--->Increased in Gln+Decreaese in Glu---->Thereafter reductions in Gln+Glu.[13]
While there is no argument that schizophrenia is associated with cognitive deficits which are in turn associated with abnormalities in the prefrontal cortex and medial temporal lobe, the fundemental cognitive processes that malfunctioning are yet to be determined. Endophenotypic and medication status-independent deficits in WM are observed in schizophrenia, regardless of the modality tested(i.e. verbal versus visual). The temporal characteristics of WM deficits in schizophrenia have led some authors to postulate that deficits are encoding related; in line with this, deficits are constant regardless of delay. However, maintence appears to be dysfunctional as well. While "hypofrontality" is a major principal in schizophenia theories, the relationship between WM task deficit appears to follow a biphasic curve, with increased dlPFC signals occuring earlier in schizophrenic patients, indicating less efficient systems of internal representation. Episodic memory also impaired, and evidence suggests that this is most prominently expressed in relational reasoning caused by hippocampal and prefrontal dysfunction. Hedonic, valenced, processing in schizophrenia appears to largely be intact, as ventral-striatal responses and subjective "liking" is not diminished, although loss-avoidance responsivity is impaired. Despite the aforementioned findings, increased anhedonia(negative symptoms) have also been reportedly associated with reduced striatal responsiveness to rewards. While basal ganglia dysfuncton is present in schizophrenia, simple reinforcement learning is not impaired. However, when reinforcement learning paradigms increase in complexity, impairment becomes apparent. While these impairments are fairly consistent, whether or the deficit is a result of online processing mechanisms(e.g. dlPFC mediated WM), associative processes, or both, is unknown. Monetary incentive delay tasks, assesing desire or "wanting" is frequently associated with reduced ventral striatal signaling in schizophrenia. This has been correlated with various symptoms and symptom dimensions, including apathy and negative symptoms in both medication naive and medicated patients. Reduced prediction errors have also been observed.
- Overall, a failure of on line maintence and reward associativty is thought to lead to impairment in the generation of cognition and behavior recquired to obtain rewads, despite normal hedonic responses.[14] From a longitudinal standpoint, deficits in verbal, nonverbal and mathematical, tests scores have been observed in people who go on to develop schizophrenia. Attentional deficits has the ability to identify which children of parents with schizophrenia will and wont go on to develop the disease themselves. One study examining the Iowa test found that deficits were only significant after the onset of puberty in those who went on to develop the disease in adulthood. [15]
Neuropathological studies suggest that volumetric deficits in the temporal lobes, prefrontal lobes, and subiculum of those with Schizophrenia can be better attributed to deficits in neuropil(neuronal extensions such as dendrites) rather than fewer cells. Postmortem gene expression studies have observed reductions in protein associated with myelin formation and regulation, which is congruent with the association between NRGN and DISC1 genetic polymorphisms and schizophrenia.[16] Reductions in GAD67 mRNA levels in the prefrontal cortex and general reduction in parvalbumin mRNA have been observed in schizophrenia, being most significant but not limited to prefrontal regions. The reductions in GABAergic neuronal proteins may be linked to the observed reductions of TrKB and BDNF as the latter proteins are involved in the regulation of the former. The reduction may also be linked to reduced excitation of GABAergic neurons, possible due to hypofunction of NMDA receptors.[17]
| Symptom Dimension | Regional Morphological Differences | Regional Functional Differences |
|---|---|---|
| Negative Symptoms |
|
|
| Psychosis |
|
|
| Disorganization |
|
|
- Resting state hypofrontality.[18]
- Rediced activation in the right middle frontal gyrus, right inferior parietal lobule, and right insula during attentional tasks. Increased activation in the left insula duting memory task.[19]
- Insula, inferior frontal cortex, superior temporal gyrus, anterior cingulate cortex, medial frontal cortex, thalamus and left amygdala volume reductions. Reduced fractional anisotropy or white matter in interhemispheric fibers, anterior thalamic radiations, inferior longitudinal fasiculus, inferior frontal occipital fasiculi, cingulum and fornix.[20]
Biology of bipolar disorder
The biology of bipolar disorder is unknown. Various abnormalities in studies of brain structure and function have been demonstrated. Various theories have posited dysfunction in monoaminergic regulation, neural circuitry, and mitochondria function as underlying bipolar disorder.
Etiology
The etiology of bipolar disorder is unknown. The overall heritability of bipolar is estimated at 79%-93%, and first degree relatives of bipolar probands have a relative risk of developing bipolar around 7-10. While the heritability is high, no specific genes have been conclusively associated with bipolar, and a number of hypothesis have been posited to explain this fact. The polygenic common rare variant hypothesis suggests that a large number of risk conferring genes are carried in a population, and that a disease manifests when a person has a sufficient number of these genes. The multiple rare variant model suggests that multiple genes that are rare in the population are capable of causing a disease, and that carrying one or a few can lead to disease.
A number of genome wide associations have been reported, including CACNA1C and ODZ4. Less consistently reported loci include ANK3 and NCAN, ITIH1, ITIH3 and NEK4. Significant overlaps with schizophrenia have been reported at CACNA1C, ITIH, ANK3, and ZNF804A. This overlap is congruent with the observation that relatives of probands with schizophrenia are at higher risk for bipolar disorder and vice versa. In light of associations between bipolar and circadian abnormalities(such as decreased need for sleep and increased sleep latency), polymorphisms in the CLOCK gene have been tested for association, although findings have been inconsistent.[21] Other circadian genes associated with bipolar at relaxed significance thresholds include ARTNL, RORB, and DEC1.[22] One meta analysis reported a significant association of the short allele of the serotonin transporter, although the study was specific to european populations.[23] Two polymorphisms in the tryptophan hydroxylase 2 gene have been associated with bipolar disorder.[24]
No significant association exists for the BDNF Val66Met allele and bipolar disorder, except in a subgroup of bipolar II cases.[25]
Pathophysiology
Neuroimaging
Structural neuroimaging studies consistently report increased frequency of white matter hyperintensities in people with bipolar. However, whether or not the lesions play a causative role is unknown. It is possible that they are a result of secondary factors, such as in increased risk of cardiovascular disease in bipolar. On the other hand, the observation of reduced white matter integrity in frontal-subcortical regions makes it possible that these hyperintensities play a role dysfunction between limbic and cortical regions. Global brain volume and morphology are normal in bipolar. Regional deficits in volume have been reported in ventrolateral and dorsolateral prefrontal regions. Based on this, it has been suggested that reduced limbic regulation by prefrontal regions plays a role in bipolar. Findings related to the volume of the basal ganglia have been inconsistent.
Functional neuroimaging studies, contrary to structural studies, consistently find hyperactivation of the basal ganglia, amygdala, and thalamus. Prefrontal abnormalities are less consistently reported, although hyperactivation in the ventral prefrontal cortex is a fairly consistent finding.[26] Mania is generally associated with frontal/ventral hypoactivation, while depression is generally associated with the opposite. A degree of lateralization with regard to abnormalities has been reported, with mania being associated with the right hemisphere, and depression the left. Trait abnormalities in euthymic patients have been observed, including hypoactivity in the ventral prefrontal cortex, and hyperactvity in the amygdala.[27] Hyperactivity in the amygdala and hypoactivity in the medial and ventral prefrontal cortex during exposure to emotional stimuli has been interpreted as reflecting dysfunction in emotional regulation circuits. Increased effective connectivity between the amygdala and orbitofrontal cortex, and elevated striatal responsiveness during reward tasks have been interpreted as hyper-responsiveness in positive emotion and reward circuitry. The abnormal activity in these circuits has been observed in non-emotional tasks, and is congruent with changes in grey and white matter in these circuits.[28] Neural response during reward tasks differentiates unipolar depression from bipolar depression, with the former being associated with reduced neural response and the latter being associated with elevated neural response.[29]
Meta analyses of structural neuroimaging studies have reported reductions in fronto-insula cortices, the anterior cingulate cortex,[30] ventricular enlargement,[31] increased volumes of the globus pallidus and increased amygdala volume relative to those with schizophrenia,[32] and reduced grey matter in the claustrum and temporal cortex.[33] A significant overlap of bipolar disorder with schizophrenia in grey matter volume reduction occurs in the anterior cingulate cortex, medial prefrontal cortex, lateral prefrontal cortex and bilateral insula.[34]
Regardless of mood state, during response inhibition tasks, people with bipolar disorder underactivate the right inferior frontal gyrus. Changes specific on euthymia include hyperactivations in the left superior temporal gyrus and hypoactivations in the basal ganglia, and changes specific to mania include hyperactivation in the basal ganglia.[35] A meta analysis of fMRI studies reported underactivations in the inferior frontal gyrus and putamen and hyperactivation of the parahippocampus, hippocampus, and amygdala. State specific abnormalities were reported for mania and euthymia. During mania, hypoactivation was significant in the inferior frontal gyrus, while euthymia was associated wit hypoactivation of the lingual gyrus and hyperactivation of the amygdala.[36]
Neurometabolites
Increased combined glutamine and glutamate(Glx) have been observed globally, regardless of medication status.[37] Increased Glx has been associated with reduced frontal mismatch negativity, interpreted as dysfunction in NMDA signaling.[38] N-acetyl aspartate levels in the basal ganglia are reduced in bipolar disorder, and trends towards increased in the dorsolateral prefrontal cortex. NAA to creatine ratios are reduced in the hippocampus.[39]
Neurochemistry
Various hypotheses related to monoamines have been proposed. The biogenic amine hypothesis posits general dysregulation of monoamines underlies bipolar and affective disorders. The cholinergic aminergic balance hypothesis posits that an increased ratio of cholingeric activity relative to adrenergic signaling underlies depression, while increased adrenergic signaling relative to cholinergic signaling underlies mania. The permissive hypothesis suggests that serotonin is necessary but not sufficient for affective symptoms, and that reduced serotonergic tone is common to both depression and mania.[40]
Studies of the binding potential of Dopamine receptor D2 and dopamine transporter have been inconsistent but Dopamine receptor D1's binding potential has been observed to be decreased, interpreted as reflecting increased synaptic dopamine in mania. Drugs that release dopamine produce effects similar to mania, further supporting the hypothesis of increase catecholaminergic activity in mania. The binding potential of muscarinic receptors are reduced in vivo during depression, as well as in post mortem studies, supporting the cholinergic aminergic balance hypothesis.[41]
Further evidence for monoamine dysfunction in bipolar comes on studies of neurotransmitter metabolites. Reduced concentration of homovallinic acid, the primary metabolite of dopamine, in the cerebrospinal fluid(CSF) of people with depression is consistently reported. This finding is related to psychomotor retardation and anhedonia. Furthermore, parkinson's disease is associated with high rates of depression, and one case study has reported the abolishment of parkinson's symptoms during manic episodes. The binding potential of VMAT2 is also elevated in bipolar I patients with a history of psychosis, although this finding is inconsistent with finding that valproate increases VMAT2 expression in rodents.[42]
Studies of serotonin's primary metabolite 5-HIAA have been inconsistent,[43] although limited evidence points towards reduced central serotonin signaling in a subgroup of aggressive or suicidal patients.[42] Studies assessing the binding potential of the serotonin transporter or serotonin receptors have also been inconsistent, but generally point towards abnormal serotonin signalling.[44]
Bipolar disorder is associated with elevated basal and dexamethasone elicited cortisol and Adrenocorticotropic hormone(ACTH). These abnormalities are particularly prominent in mania, and are inversely associated with antipsychotic use.[45]
Intracellular Signaling
The levels of Gαs but not other g proteins is increased in the frontal, temporal and occipital cortices. The binding of serotonin receptors to g proteins is also elevated globally. Leukocyte and platelet levels of Gαs and Gαi is also elavated in those with bipolar disorder. Downstream targets of g protein signaling is also altered in bipolar disorder. Increased levels of adenylyl cyclase, protein kinase A(PKA), and cyclic adenosine monophosphate induced PKA activity is also elevated. Phosphoinositide signaling is also altered, with elevated levels of phospholipase C, protein kinase C, and Gαq being reported in bipolar.[46]
Glycogen synthase kinase 3 has been implicated in bipolar disorder, as bipolar medications lithium and valproate have been shown to increase ints phosphorylation, thereby inhibiting it. However, postmortem studies hvae not shown any differences in GSK-3 levels or the levels of a downstream target β-catenin.[47]
Mitochondrial Dysfunction
Some researchers have suggested bipolar disorder is a mitochondrial disease. Some cases of familial chronic progressive external ophthalmoplegia demonstrate increased rates of bipolar disorder before the onset of CPEO, and the higher rate of maternal inheritance patterns support this hypothesis. Further support this hypothesis is the abnormal findings in magnetic resonance spectroscopy studies of brain metabolites in people with bipolar.[48]
Neuropathology
A number of abnormalities in GABAergic neurons have been reported in people with bipolar disorder. People with bipolar demonstrate reduced expression of GAD67 in CA3/CA2 subregion of the hippocampus. More extensive reductions of other indicators of GABA function have been reported in in the CA4 and CA1. Abnormal expression of kainate receptors on GABAergic cells have been reported, with reductions in GRIK1 and GRIK2 mRNA in the CA2/CA3 being found in people with bipolar. Decreased levels of HCN channels have also been reported, which, along with abnormal glutamate signaling, could contribute to reduced GABAergic tone in the hippocampus.[49]
The observation of increased Glx in the prefrontal cortex is congruent with the observation of reduced glial cell counts and prefrontal cortex volume, as glia play an important role in glutamate homeostasis.[50]
Immune Dysfunction
Elevated levels of IL-6, C-reactive protein(CRP) and TNFα have been reported in bipolar. Levels of some(IL-6 and CRP) but not all (TNFα) may be reduced by treatment. Increases in IL-6 have been reported in mood episodes, regardless of polarity.[51]
Sources to Integrate
Reviews
Bipolar
- Meta-analysis of regional white matter volume in bipolar disorder with replication in an independent sample using coordinates, T-maps, and individual MRI data.
- The dopamine hypothesis of bipolar affective disorder: the state of the art and implications for treatmen
- Neurobiological underpinnings of bipolar disorder focusing on findings of diffusion tensor imaging: a systematic review
- DTI and Myelin Plasticity in Bipolar Disorder: Integrating Neuroimaging and Neuropathological Findings
- Biomarkers and staging of bipolar disorder: a systematic review
- The Kraepelinian dichotomy viewed by neuroimaging
- A review of MR spectroscopy studies of pediatric bipolar disorder.
- Assessing working memory via N-back task in euthymic bipolar I disorder patients: a review of functional magnetic resonance imaging studies.
- Overlapping prefrontal systems involved in cognitive and emotional processing in euthymic bipolar disorder and following sleep deprivation: a review of functional neuroimaging studies.
- Mechanistic comparisons of functional domains across pediatric and adult bipolar disorder highlight similarities, as well as differences, influenced by the developing brain.
- Neurocognitive and neuroimaging predictors of clinical outcome in bipolar disorder.
- Bipolar disorder: from genes to behavior pathways.
- A neural model of voluntary and automatic emotion regulation: implications for understanding the pathophysiology and neurodevelopment of bipolar disorder.
- Neuroimaging in bipolar disorder: a critical review of current findings.
- In vivo imaging of synaptic function in the central nervous system: II. Mental and affective disorders.
Obsessive-compulsive disorder
Meta analyses
Bipolar
- Voxel-Based Meta-Analytical Evidence of Structural Disconnectivity in Major Depression and Bipolar Disorder
- Evidence of diagnostic specificity in the neural correlates of facial affect processing in bipolar disorder and schizophrenia: a meta-analysis of functional imaging studies
- Structural neuroimaging studies in major depressive disorder. Meta-analysis and comparison with bipolar disorder
- Toward a functional neuroanatomical signature of bipolar disorder: quantitative evidence from the neuroimaging literature
- A meta-analysis of whole-brain diffusion tensor imaging studies in bipolar disorder.
- Neuroimaging-based markers of bipolar disorder: evidence from two meta-analyses.
- Gray matter, white matter, brain, and intracranial volumes in first-episode bipolar disorder: a meta-analysis of magnetic resonance imaging studies
- Meta-analysis of amygdala volumes in children and adolescents with bipolar disorder
- Fronto-limbic brain abnormalities in juvenile onset bipolar disorder
- Meta-analysis of magnetic resonance imaging brain morphometry studies in bipolar disorder
- Systematic review and voxel-based meta-analysis of diffusion tensor imaging studies in bipolar disorder.
Obsessive-compulsive disorder
MDD
| Link | Decreases(-) | Increases(+) | Measure |
|---|---|---|---|
| Kühn 2013
Resting-state brain activity in schizophrenia and major depression: a quantitative meta-analysis. |
|
|
Resting activity |
| Miller 2015 |
Functional activity | ||
| Wang 2016
Serotonin-1A receptor alterations in depression: a meta-analysis of molecular imaging studies |
|
5-HT1A receptor BP | |
| Du 2012
Voxelwise meta-analysis of gray matter reduction in major depressive disorder |
|
Grey matter volume | |
| Hamilton 2012 |
|
|
Functional activity |
| Zhang 2016 |
|
Grey matter volume | |
| Bora 2012 |
|
Grey matter | |
| Lai 2013
Gray matter volume in major depressive disorder: a meta-analysis of voxel-based morphometry studies |
|
Grey matter | |
| Sacher 2012 |
|
|
Decreases(GMV), increases(Glucose metebolism) |
| Gryglewski 2014
Meta-analysis of molecular imaging of serotonin transporters in major depression |
|
5-HTT Binding potential |
Various Shenanigans
| Title | Year | Disorder | Papers(n) | Subjects | Pubmed Link | Full Text Link | Full Text Link | DOI | Increased Activity, GM, WM or BP | Reduced Activity, GM, WM OR BP | Conclusion | Average Subjects |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Functional Decoding and Meta-analytic Connectivity Modeling in Adult Attention-Deficit/Hyperactivity Disorder. | 2016 | ADHD | 24 | - | https://www.ncbi.nlm.nih.gov/pubmed/27569542 | sci-hub.tw/10.1016/j.biopsych.2016.06.014. | sci-hub.la/10.1016/j.biopsych.2016.06.014. | 10.1016/j.biopsych.2016.06.014. | L PUT, L IFG, R CAUD | - | ||
| A systematic review and meta-analysis of tract-based spatial statistics studies regarding attention-deficit/hyperactivity disorder | 2016 | ADHD | 10 | 947 | https://www.ncbi.nlm.nih.gov/pubmed/27450582 | sci-hub.tw/10.1016/j.neubiorev.2016.07.022 | sci-hub.la/10.1016/j.neubiorev.2016.07.022 | 10.1016/j.neubiorev.2016.07.022 | - | SS, Sagital Stratum | 94.7 | |
| Striatal dopamine transporter alterations in ADHD: pathophysiology or adaptation to psychostimulants? A meta-analysis. | 2012 | ADHD | 9 | 169 | https://www.ncbi.nlm.nih.gov/pubmed/22294258 | sci-hub.tw/10.1176/appi.ajp.2011.11060940. | sci-hub.la/10.1176/appi.ajp.2011.11060940. | 10.1176/appi.ajp.2011.11060940. | Striatal DAT | - | 18.8 | |
| Toward systems neuroscience of ADHD: a meta-analysis of 55 fMRI studies. | 2012 | ADHD | 55 | 1542 | https://www.ncbi.nlm.nih.gov/pubmed/22983386 | sci-hub.tw/10.1176/appi.ajp.2012.11101521. | sci-hub.la/10.1176/appi.ajp.2012.11101521. | 10.1176/appi.ajp.2012.11101521. | MCC, Angular | R vlPFC, L INS, L PUT | 28.0 | |
| Diffusion tensor imaging in attention deficit/hyperactivity disorder: a systematic review and meta-analysis | 2012 | ADHD | 9 | 342 | https://www.ncbi.nlm.nih.gov/pubmed/22305957 | sci-hub.tw/10.1016/j.neubiorev.2012.01.003 | sci-hub.la/10.1016/j.neubiorev.2012.01.003 | 10.1016/j.neubiorev.2012.01.003 | 38.0 | |||
| Meta-analysis of structural MRI studies in children and adults with attention deficit hyperactivitydisorder indicates treatment effects | 2012 | ADHD | 11 | 608 | https://www.ncbi.nlm.nih.gov/pubmed/22118249 | sci-hub.tw/10.1111/j.1600-0447.2011.01786.x | sci-hub.la/10.1111/j.1600-0447.2011.01786.x | 10.1111/j.1600-0447.2011.01786.x | 55.3 | |||
| Gray matter volume abnormalities in ADHD: voxel-based meta-analysis exploring the effects of age and stimulant medication | 2011 | ADHD | 14 | 622 | https://www.ncbi.nlm.nih.gov/pubmed/21865529 | sci-hub.tw/10.1176/appi.ajp.2011.11020281 | sci-hub.la/10.1176/appi.ajp.2011.11020281 | 10.1176/appi.ajp.2011.11020281 | 44.4 | |||
| Structural Neuroimaging of Anorexia Nervosa: Future Directions in the Quest for Mechanisms Underlying Dynamic Alterations. | 2018 | AN | - | - | https://www.ncbi.nlm.nih.gov/pubmed/28967386 | sci-hub.tw/10.1016/j.biopsych.2017.08.011 | sci-hub.la/10.1016/j.biopsych.2017.08.011 | 10.1016/j.biopsych.2017.08.011 | - | |||
| Behind binge eating: A review of food-specific adaptations of neurocognitive and neuroimaging tasks. | 2017 | AN | - | - | https://www.ncbi.nlm.nih.gov/pubmed/28363840 | sci-hub.tw/10.1016/j.physbeh.2017.03.037 | sci-hub.la/10.1016/j.physbeh.2017.03.037 | 10.1016/j.physbeh.2017.03.037 | - | |||
| Functional brain alterations in anorexia nervosa: a scoping review. | 2016 | AN | 49 | - | https://www.ncbi.nlm.nih.gov/pubmed/27933159 | sci-hub.tw/10.1186/s40337-016-0118-y | sci-hub.la/10.1186/s40337-016-0118-y | 10.1186/s40337-016-0118-y | - | |||
| A systematic review of resting-state functional-MRI studies in anorexia nervosa: Evidence for functional connectivity impairment in cognitive control and visuospatial and body-signal integration. | 2016 | AN | 15 | 294 | https://www.ncbi.nlm.nih.gov/pubmed/27725172 | sci-hub.tw/10.1016/j.neubiorev.2016.09.032 | sci-hub.la/10.1016/j.neubiorev.2016.09.032 | 10.1016/j.neubiorev.2016.09.032 | 19.6 | |||
| Brain morphological changes in adolescent and adult patients with anorexia nervosa. | 2016 | AN | 29 | 273 | https://www.ncbi.nlm.nih.gov/pubmed/27188331 | sci-hub.tw/10.1007/s00702-016-1567-9 | sci-hub.la/10.1007/s00702-016-1567-9 | 10.1007/s00702-016-1567-9 | 9.4 | |||
| Morphological changes in the brain of acutely ill and weight-recovered patients with anorexia nervosa. A meta-analysis and qualitative review. | 2014 | AN | - | 177 | https://www.ncbi.nlm.nih.gov/pubmed/24365959 | sci-hub.tw/10.1024/1422-4917/a000265 | sci-hub.la/10.1024/1422-4917/a000265 | 10.1024/1422-4917/a000265 | - | |||
| Anorexia nervosa is linked to reduced brain structure in reward and somatosensory regions: a meta-analysis of VBM studies. | 2013 | AN | 9 | 228 | https://www.ncbi.nlm.nih.gov/pubmed/23570420 | sci-hub.tw/10.1186/1471-244X-13-110 | sci-hub.la/10.1186/1471-244X-13-110 | 10.1186/1471-244X-13-110 | 25.3 | |||
| Neural basis of a multidimensional model of body image distortion in anorexia nervosa. | 2012 | AN | - | - | https://www.ncbi.nlm.nih.gov/pubmed/22613629 | sci-hub.tw/10.1016/j.neubiorev.2012.05.003 | sci-hub.la/10.1016/j.neubiorev.2012.05.003 | 10.1016/j.neubiorev.2012.05.003 | - | |||
| Processing of food, body and emotional stimuli in anorexia nervosa: a systematic review and meta-analysis of functional magnetic resonance imaging studies. | 2012 | AN | 15 | - | https://www.ncbi.nlm.nih.gov/pubmed/22945872 | sci-hub.tw/10.1002/erv.2197 | sci-hub.la/10.1002/erv.2197 | 10.1002/erv.2197 | - | |||
| The common traits of the ACC and PFC in anxiety disorders in the DSM-5: meta-analysis of voxel-based morphometry studies. | 2014 | ANX | 24 | 1264 | https://www.ncbi.nlm.nih.gov/pubmed/24676455 | sci-hub.tw/10.1371/journal.pone.0093432 | sci-hub.la/10.1371/journal.pone.0093432 | 10.1371/journal.pone.0093432 | 52.7 | |||
| Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. | 2007 | ANX | 19 | 1674 | https://www.ncbi.nlm.nih.gov/pubmed/17898336 | sci-hub.tw/10.1176/appi.ajp.2007.07030504 | sci-hub.la/10.1176/appi.ajp.2007.07030504 | 10.1176/appi.ajp.2007.07030504 | 88.1 | |||
| Prefrontal Structural and Functional Brain Imaging findings in Antisocial, Violent, and Psychopathic Individuals: A Meta-Analysis | 2009 | ASPD | 43 | 1262 | https://www.ncbi.nlm.nih.gov/pubmed/19833485 | sci-hub.tw/10.1016/j.pscychresns.2009.03.012 | sci-hub.la/10.1016/j.pscychresns.2009.03.012 | 10.1016/j.pscychresns.2009.03.012 | 29.3 | |||
| Neuroimaging in bulimia nervosa and binge eating disorder: a systematic review. | 2018 | BN | 32 | - | https://www.ncbi.nlm.nih.gov/pubmed/29468065 | sci-hub.tw/10.1186/s40337-018-0187-1 | sci-hub.la/10.1186/s40337-018-0187-1 | 10.1186/s40337-018-0187-1 | - | |||
| Inhibitory control in obesity and binge eating disorder: A systematic review and meta-analysis of neurocognitive and neuroimaging studies. | 2016 | BN | 8 | 150 | https://www.ncbi.nlm.nih.gov/pubmed/27381956 | sci-hub.tw/10.1016/j.neubiorev.2016.06.041 | sci-hub.la/10.1016/j.neubiorev.2016.06.041 | 10.1016/j.neubiorev.2016.06.041 | 18.8 | |||
| Common and distinct patterns of grey-matter volume alteration in major depression and bipolar disorder: evidence from voxel-based meta-analysis. | 2017 | BP | 86 | 6058 | https://www.ncbi.nlm.nih.gov/pubmed/27217146 | sci-hub.tw/10.1038/mp.2016.72 | sci-hub.la/10.1038/mp.2016.72 | 10.1038/mp.2016.72 | S dmPFC | pgACC, sgACC, INS | 70.4 | |
| Meta-analysis of functional magnetic resonance imaging studies of timing and cognitive control in schizophrenia and bipolar disorder: Evidence of a primary time deficit. | 2017 | BP | 22 | 772 | https://www.ncbi.nlm.nih.gov/pubmed/28169089 | sci-hub.tw/10.1016/j.schres.2017.01.039 | sci-hub.la/10.1016/j.schres.2017.01.039 | 10.1016/j.schres.2017.01.039 | 35.1 | |||
| Brain functional effects of psychopharmacological treatments in bipolar disorder. | 2016 | BP | 140 | - | https://www.ncbi.nlm.nih.gov/pubmed/27617780 | sci-hub.tw/10.1016/j.euroneuro.2016.06.006 | sci-hub.la/10.1016/j.euroneuro.2016.06.006 | 10.1016/j.euroneuro.2016.06.006 | - | |||
| Subcortical volumetric abnormalities in bipolar disorder. | 2016 | BP | 1 | 4304 | https://www.ncbi.nlm.nih.gov/pubmed/26857596 | sci-hub.tw/10.1038/mp.2015.227 | sci-hub.la/10.1038/mp.2015.227 | 10.1038/mp.2015.227 | 4304.0 | |||
| Voxel-Based Meta-Analytical Evidence of Structural Disconnectivity in Major Depression and Bipolar Disorder. | 2016 | BP | 40 | 2429 | https://www.ncbi.nlm.nih.gov/pubmed/25891219 | sci-hub.tw/10.1016/j.biopsych.2015.03.004 | sci-hub.la/10.1016/j.biopsych.2015.03.004 | 10.1016/j.biopsych.2015.03.004 | 60.7 | |||
| A critical appraisal of neuroimaging studies of bipolar disorder: toward a new conceptualization of underlying neural circuitry and a road map for future research. | 2014 | BP | - | - | https://www.ncbi.nlm.nih.gov/pubmed/24626773 | sci-hub.tw/10.1176/appi.ajp.2014.13081008 | sci-hub.la/10.1176/appi.ajp.2014.13081008 | 10.1176/appi.ajp.2014.13081008 | - | |||
| Elevated reward-related neural activation as a unique biological marker of bipolar disorder: assessment and treatment implications. | 2014 | BP | - | - | https://www.ncbi.nlm.nih.gov/pubmed/25241675 | sci-hub.tw/10.1016/j.brat.2014.08.011 | sci-hub.la/10.1016/j.brat.2014.08.011 | 10.1016/j.brat.2014.08.011 | - | |||
| Developmental meta-analyses of the functional neural correlates of bipolar disorder. | 2014 | BP | 94 | 3896 | https://www.ncbi.nlm.nih.gov/pubmed/25100166 | sci-hub.tw/10.1001/jamapsychiatry.2014.660 | sci-hub.la/10.1001/jamapsychiatry.2014.660 | 10.1001/jamapsychiatry.2014.660 | 41.4 | |||
| Could glutamate spectroscopy differentiate bipolar depression from unipolar? | 2014 | BP | 11 | 431 | https://www.ncbi.nlm.nih.gov/pubmed/25082118 | sci-hub.tw/10.1016/j.jad.2014.05.019 | sci-hub.la/10.1016/j.jad.2014.05.019 | 10.1016/j.jad.2014.05.019 | 39.2 | |||
| Gray matter abnormalities as brain structural vulnerability factors for bipolar disorder: A review of neuroimaging studies of individuals at high genetic risk for bipolar disorder. | 2013 | BP | - | - | https://www.ncbi.nlm.nih.gov/pubmed/23864160 | sci-hub.tw/10.1177/0004867413496482 | sci-hub.la/10.1177/0004867413496482 | 10.1177/0004867413496482 | - | |||
| Functional neuroanatomy of response inhibition in bipolar disorders--combined voxel based and cognitive performance meta-analysis. | 2013 | BP | 30 | 1302 | https://www.ncbi.nlm.nih.gov/pubmed/24070910 | sci-hub.tw/10.1016/j.jpsychires.2013.08.015 | sci-hub.la/10.1016/j.jpsychires.2013.08.015 | 10.1016/j.jpsychires.2013.08.015 | 43.4 | |||
| Evidence of diagnostic specificity in the neural correlates of facial affect processing in bipolar disorder and schizophrenia: a meta-analysis of functional imaging studies. | 2013 | BP | 29 | 750 | https://www.ncbi.nlm.nih.gov/pubmed/22874625 | sci-hub.tw/10.1017/S0033291712001432 | sci-hub.la/10.1017/S0033291712001432 | 10.1017/S0033291712001432 | 25.9 | |||
| A systematic review and meta-analysis of proton magnetic resonance spectroscopy and mismatch negativity in bipolar disorder. | 2013 | BP | 15 | 368 | https://www.ncbi.nlm.nih.gov/pubmed/23968965 | sci-hub.tw/10.1016/j.euroneuro.2013.07.007 | sci-hub.la/10.1016/j.euroneuro.2013.07.007 | 10.1016/j.euroneuro.2013.07.007 | 24.5 | |||
| Mapping vulnerability to bipolar disorder: a systematic review and meta-analysis of neuroimaging studies. | 2012 | BP | 37 | 2254 | https://www.ncbi.nlm.nih.gov/pubmed/22297067 | sci-hub.tw/10.1503/jpn.110061 | sci-hub.la/10.1503/jpn.110061 | 10.1503/jpn.110061 | 60.9 | |||
| Neurometabolites in schizophrenia and bipolar disorder - a systematic review and meta-analysis. | 2012 | BP | 43 | 1461 | https://www.ncbi.nlm.nih.gov/pubmed/22981426 | sci-hub.tw/10.1016/j.pscychresns.2012.02.003 | sci-hub.la/10.1016/j.pscychresns.2012.02.003 | 10.1016/j.pscychresns.2012.02.003 | 34.0 | |||
| Common and distinct neural correlates of emotional processing in Bipolar Disorder and Major Depressive Disorder: a voxel-based meta-analysis of functional magnetic resonance imaging studies. | 2012 | BP | 20 | 701 | https://www.ncbi.nlm.nih.gov/pubmed/21820878 | sci-hub.tw/10.1016/j.euroneuro.2011.07.003 | sci-hub.la/10.1016/j.euroneuro.2011.07.003 | 10.1016/j.euroneuro.2011.07.003 | 35.1 | |||
| Grey matter differences in bipolar disorder: a meta-analysis of voxel-based morphometry studies. | 2012 | BP | 8 | 520 | https://www.ncbi.nlm.nih.gov/pubmed/22420589 | sci-hub.tw/10.1111/j.1399-5618.2012.01000.x | sci-hub.la/10.1111/j.1399-5618.2012.01000.x | 10.1111/j.1399-5618.2012.01000.x | 65.0 | |||
| A quantitative meta-analysis of fMRI studies in bipolar disorder. | 2011 | BP | 65 | 2114 | https://www.ncbi.nlm.nih.gov/pubmed/21320248 | sci-hub.tw/10.1111/j.1399-5618.2011.00893.x | sci-hub.la/10.1111/j.1399-5618.2011.00893.x | 10.1111/j.1399-5618.2011.00893.x | 32.5 | |||
| Toward a functional neuroanatomical signature of bipolar disorder: quantitative evidence from the neuroimaging literature. | 2011 | BP | 55 | 1584 | https://www.ncbi.nlm.nih.gov/pubmed/21676596 | sci-hub.tw/10.1016/j.pscychresns.2011.02.011 | sci-hub.la/10.1016/j.pscychresns.2011.02.011 | 10.1016/j.pscychresns.2011.02.011 | 28.8 | |||
| Neuroimaging-based markers of bipolar disorder: evidence from two meta-analyses. | 2011 | BP | 28 | 1561 | https://www.ncbi.nlm.nih.gov/pubmed/21470688 | sci-hub.tw/10.1016/j.jad.2011.03.016 | sci-hub.la/10.1016/j.jad.2011.03.016 | 10.1016/j.jad.2011.03.016 | 55.8 | |||
| Voxelwise meta-analysis of gray matter abnormalities in bipolar disorder. | 2010 | BP | 21 | 1430 | https://www.ncbi.nlm.nih.gov/pubmed/20303066 | sci-hub.tw/10.1016/j.biopsych.2010.01.020 | sci-hub.la/10.1016/j.biopsych.2010.01.020 | 10.1016/j.biopsych.2010.01.020 | 68.1 | |||
| Correlation between amygdala volume and age in bipolar disorder - a systematic review and meta-analysis of structural MRI studies. | 2010 | BP | 13 | 877 | https://www.ncbi.nlm.nih.gov/pubmed/20226638 | sci-hub.tw/10.1016/j.pscychresns.2009.09.004 | sci-hub.la/10.1016/j.pscychresns.2009.09.004 | 10.1016/j.pscychresns.2009.09.004 | 67.5 | |||
| Magnetic resonance imaging studies in bipolar disorder and schizophrenia: meta-analysis. | 2009 | BP | 65 | 1384 | https://www.ncbi.nlm.nih.gov/pubmed/19721106 | sci-hub.tw/10.1192/bjp.bp.108.059717 | sci-hub.la/10.1192/bjp.bp.108.059717 | 10.1192/bjp.bp.108.059717 | 21.3 | |||
| Meta-analysis, database, and meta-regression of 98 structural imaging studies in bipolar disorder. | 2008 | BP | 98 | 8196 | https://www.ncbi.nlm.nih.gov/pubmed/18762588 | sci-hub.tw/10.1001/archpsyc.65.9.1017 | sci-hub.la/10.1001/archpsyc.65.9.1017 | 10.1001/archpsyc.65.9.1017 | 83.6 | |||
| Meta-analysis of amygdala volumes in children and adolescents with bipolar disorder. | 2008 | BP | 11 | 553 | https://www.ncbi.nlm.nih.gov/pubmed/18827720 | sci-hub.tw/10.1097/CHI.0b013e318185d299 | sci-hub.la/10.1097/CHI.0b013e318185d299 | 10.1097/CHI.0b013e318185d299 | 50.3 | |||
| Neurochemical alterations of the brain in bipolar disorder and their implications for pathophysiology: a systematic review of the in vivo proton magnetic resonance spectroscopy findings. | 2006 | BP | - | - | https://www.ncbi.nlm.nih.gov/pubmed/16677749 | sci-hub.tw/10.1016/j.pnpbp.2006.03.012 | sci-hub.la/10.1016/j.pnpbp.2006.03.012 | 10.1016/j.pnpbp.2006.03.012 | - | |||
| Neural Correlates of Disturbed Emotion Processing in Borderline Personality Disorder: A Multimodal Meta-Analysis. | 2016 | BPD | 29 | 1115 | https://www.ncbi.nlm.nih.gov/pubmed/25935068 | sci-hub.tw/10.1016/j.biopsych.2015.03.027 | sci-hub.la/10.1016/j.biopsych.2015.03.027 | 10.1016/j.biopsych.2015.03.027 | 38.4 | |||
| Mapping the brain correlates of borderline personality disorder: A functional neuroimaging meta-analysis of resting state studies. | 2016 | BPD | 7 | 299 | https://www.ncbi.nlm.nih.gov/pubmed/27552444 | sci-hub.tw/10.1016/j.jad.2016.07.025 | sci-hub.la/10.1016/j.jad.2016.07.025 | 10.1016/j.jad.2016.07.025 | 42.7 | |||
| Meta-analysis of molecular imaging of serotonin transporters in ecstasy/polydrug users. | 2016 | DA | 7 | 305 | https://www.ncbi.nlm.nih.gov/pubmed/26855234 | sci-hub.tw/10.1016/j.neubiorev.2016.02.003 | sci-hub.la/10.1016/j.neubiorev.2016.02.003 | 10.1016/j.neubiorev.2016.02.003 | 43.6 | |||
| A Systematic Review and Meta-analysis of Neuroimaging in Oppositional Defiant Disorder (ODD) and Conduct Disorder (CD) Taking Attention-Deficit Hyperactivity Disorder (ADHD) Into Account. | 2016 | DBD | 29 | 838 | https://www.ncbi.nlm.nih.gov/pubmed/26846227 | sci-hub.tw/10.1007/s11065-015-9315-8 | sci-hub.la/10.1007/s11065-015-9315-8 | 10.1007/s11065-015-9315-8 | 28.9 | |||
| Meta-Analysis of fMRI Studies of Disruptive Behavior Disorders. | 2016 | DBD | 24 | 636 | https://www.ncbi.nlm.nih.gov/pubmed/27523497 | sci-hub.tw/10.1176/appi.ajp.2016.15081089 | sci-hub.la/10.1176/appi.ajp.2016.15081089 | 10.1176/appi.ajp.2016.15081089 | 26.5 | |||
| Alterations in emotion generation and regulation neurocircuitry in depression and eating disorders: A comparative review of structural and functional neuroimaging studies. | 2016 | ED | - | - | https://www.ncbi.nlm.nih.gov/pubmed/27422451 | sci-hub.tw/10.1016/j.neubiorev.2016.07.011 | sci-hub.la/10.1016/j.neubiorev.2016.07.011 | 10.1016/j.neubiorev.2016.07.011 | - | |||
| A systematic review of temporal discounting in eating disorders and obesity: Behavioural and neuroimaging findings. | 2016 | ED | 31 | 4546 | https://www.ncbi.nlm.nih.gov/pubmed/27693228 | sci-hub.tw/10.1016/j.neubiorev.2016.09.024 | sci-hub.la/10.1016/j.neubiorev.2016.09.024 | 10.1016/j.neubiorev.2016.09.024 | 146.6 | |||
| Neuroimaging and neuromodulation approaches to study eating behavior and prevent and treat eating disorders and obesity. | 2015 | ED | - | - | https://www.ncbi.nlm.nih.gov/pubmed/26110109 | sci-hub.tw/10.1016/j.nicl.2015.03.016 | sci-hub.la/10.1016/j.nicl.2015.03.016 | 10.1016/j.nicl.2015.03.016 | - | |||
| Positron emission tomography studies in eating disorders: multireceptor brain imaging, correlates with behavior and implications for pharmacotherapy. | 2005 | ED | - | - | https://www.ncbi.nlm.nih.gov/pubmed/16243652 | sci-hub.tw/10.1016/j.nucmedbio.2005.06.011 | sci-hub.la/10.1016/j.nucmedbio.2005.06.011 | 10.1016/j.nucmedbio.2005.06.011 | - | |||
| Melancholy, anhedonia, apathy: the search for separable behaviors and neural circuits in depression. | 2018 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/29529482 | sci-hub.tw/10.1016/j.conb.2018.02.018 | sci-hub.la/10.1016/j.conb.2018.02.018 | 10.1016/j.conb.2018.02.018 | - | |||
| Circuit-based frameworks of depressive behaviors: The role of reward circuitry and beyond. | 2018 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/29309799 | sci-hub.tw/10.1016/j.pbb.2017.12.010 | sci-hub.la/10.1016/j.pbb.2017.12.010 | 10.1016/j.pbb.2017.12.010 | - | |||
| Treatment resistant depression: A multi-scale, systems biology approach. | 2018 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/28859997 | sci-hub.tw/10.1016/j.neubiorev.2017.08.019 | sci-hub.la/10.1016/j.neubiorev.2017.08.019 | 10.1016/j.neubiorev.2017.08.019 | - | |||
| Dopamine System Dysregulation in Major Depressive Disorders. | 2018 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/29106542 | sci-hub.tw/10.1093/ijnp/pyx056 | sci-hub.la/10.1093/ijnp/pyx056 | 10.1093/ijnp/pyx056 | - | |||
| Progress in understanding mood disorders: optogenetic dissection of neural circuits. | 2018 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/23682971 | sci-hub.tw/10.1111/gbb.12049 | sci-hub.la/10.1111/gbb.12049 | 10.1111/gbb.12049 | - | |||
| Presentation and Neurobiology of Anhedonia in Mood Disorders: Commonalities and Distinctions. | 2018 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/29520717 | sci-hub.tw/10.1007/s11920-018-0877-z | sci-hub.la/10.1007/s11920-018-0877-z | 10.1007/s11920-018-0877-z | - | |||
| Lateral habenula in the pathophysiology of depression. | 2018 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/29175713 | sci-hub.tw/10.1016/j.conb.2017.10.024 | sci-hub.la/10.1016/j.conb.2017.10.024 | 10.1016/j.conb.2017.10.024 | - | |||
| Neuroimaging genomic studies in major depressive disorder: A systematic review. | 2018 | MDD | 64 | - | https://www.ncbi.nlm.nih.gov/pubmed/29476595 | sci-hub.tw/10.1111/cns.12829 | sci-hub.la/10.1111/cns.12829 | 10.1111/cns.12829 | - | |||
| Cortical abnormalities in adults and adolescents with major depression based on brain scans from 20 cohorts worldwide in the ENIGMA Major Depressive Disorder Working Group. | 2017 | MDD | 20 | 10105 | https://www.ncbi.nlm.nih.gov/pubmed/27137745 | sci-hub.tw/10.1038/mp.2016.60 | sci-hub.la/10.1038/mp.2016.60 | 10.1038/mp.2016.60 | 505.3 | |||
| Subcortical brain structure and suicidal behaviour in major depressive disorder: a meta-analysis from the ENIGMA-MDD working group. | 2017 | MDD | 1 | 3097 | https://www.ncbi.nlm.nih.gov/pubmed/28463239 | sci-hub.tw/10.1038/tp.2017.84 | sci-hub.la/10.1038/tp.2017.84 | 10.1038/tp.2017.84 | 3097.0 | |||
| Disorganization of white matter architecture in major depressive disorder: a meta-analysis of diffusion tensor imaging with tract-based spatial statistics | 2017 | MDD | 18 | 1122 | https://www.ncbi.nlm.nih.gov/pubmed/26906716 | sci-hub.tw/10.1038/srep21825 | sci-hub.la/10.1038/srep21825 | 10.1038/srep21825 | 62.3 | |||
| Computational meta-analysis of statistical parametric maps in major depression | 2017 | MDD | 12 | 1052 | https://www.ncbi.nlm.nih.gov/pubmed/26854015 | sci-hub.tw/10.1002/hbm.23108 | sci-hub.la/10.1002/hbm.23108 | 10.1002/hbm.23108 | 87.7 | |||
| Altered Brain Activity in Unipolar Depression Revisited: Meta-analyses of Neuroimaging Studies. | 2017 | MDD | 57 | 2116 | https://www.ncbi.nlm.nih.gov/pubmed/27829086 | sci-hub.tw/10.1001/jamapsychiatry.2016.2783 | sci-hub.la/10.1001/jamapsychiatry.2016.2783 | 10.1001/jamapsychiatry.2016.2783 | 37.1 | |||
| Characterization of brain blood flow and the amplitude of low-frequency fluctuations in major depressive disorder: A multimodal meta-analysis. | 2017 | MDD | 16 | 972 | https://www.ncbi.nlm.nih.gov/pubmed/28068619 | sci-hub.tw/10.1016/j.jad.2016.12.032 | sci-hub.la/10.1016/j.jad.2016.12.032 | 10.1016/j.jad.2016.12.032 | 60.8 | |||
| Intrinsic cerebral activity at resting state in adults with major depressive disorder: A meta-analysis. | 2017 | MDD | 15 | 859 | https://www.ncbi.nlm.nih.gov/pubmed/28174129 | sci-hub.tw/10.1016/j.pnpbp.2017.02.001 | sci-hub.la/10.1016/j.pnpbp.2017.02.001 | 10.1016/j.pnpbp.2017.02.001 | 57.3 | |||
| Microstructural brain abnormalities in medication-free patients with major depressive disorder: a systematic review and meta-analysis of diffusion tensor imaging | 2017 | MDD | 15 | 864 | https://www.ncbi.nlm.nih.gov/pubmed/27780031 | sci-hub.tw/10.1503/jpn.150341 | sci-hub.la/10.1503/jpn.150341 | 10.1503/jpn.150341 | 57.6 | |||
| Corticostriatal circuitry in regulating diseases characterized by intrusive thinking. | 2016 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/27069381 | https://www.ncbi.nlm.nih.gov/pubmed/27069381 | https://www.ncbi.nlm.nih.gov/pubmed/27069381 | https://www.ncbi.nlm.nih.gov/pubmed/27069381 | - | |||
| Reward processing by the lateral habenula in normal and depressive behaviors. | 2016 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/25157511 | sci-hub.tw/10.1038/nn.3779 | sci-hub.la/10.1038/nn.3779 | 10.1038/nn.3779 | - | |||
| Subcortical brain alterations in major depressive disorder: findings from the ENIGMA Major Depressive Disorder working group. | 2016 | MDD | 1 | 8927 | https://www.ncbi.nlm.nih.gov/pubmed/26122586 | sci-hub.tw/10.1038/mp.2015.69 | sci-hub.la/10.1038/mp.2015.69 | 10.1038/mp.2015.69 | 8927.0 | |||
| Shared white matter alterations across emotional disorders: A voxel-based meta-analysis of fractional anisotropy. | 2016 | MDD | 37 | 1954 | https://www.ncbi.nlm.nih.gov/pubmed/27995068 | sci-hub.tw/10.1016/j.nicl.2016.09.001 | sci-hub.la/10.1016/j.nicl.2016.09.001 | 10.1016/j.nicl.2016.09.001 | 52.8 | |||
| Functional alterations of fronto-limbic circuit and default mode network systems in first-episode, drug-naïve patients with major depressive disorder: A meta-analysis of resting-state fMRI data. | 2016 | MDD | 31 | 908 | https://www.ncbi.nlm.nih.gov/pubmed/27639862 | sci-hub.tw/10.1016/j.jad.2016.09.005 | sci-hub.la/10.1016/j.jad.2016.09.005 | 10.1016/j.jad.2016.09.005 | 29.3 | |||
| Essential brain structural alterations in major depressive disorder: A voxel-wise meta-analysis on first episode, medication-naive patients. | 2016 | MDD | 10 | 669 | https://www.ncbi.nlm.nih.gov/pubmed/27100056 | sci-hub.tw/10.1016/j.jad.2016.04.001 | sci-hub.la/10.1016/j.jad.2016.04.001 | 10.1016/j.jad.2016.04.001 | 66.9 | |||
| Serotonin-1A receptor alterations in depression: a meta-analysis of molecular imaging studies. | 2016 | MDD | 10 | 479 | https://www.ncbi.nlm.nih.gov/pubmed/27623971 | sci-hub.tw/10.1186/s12888-016-1025-0 | sci-hub.la/10.1186/s12888-016-1025-0 | 10.1186/s12888-016-1025-0 | 47.9 | |||
| Abnormal reward functioning across substance use disorders and major depressive disorder: Considering reward as a transdiagnostic mechanism. | 2015 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/25655926 | sci-hub.tw/10.1016/j.ijpsycho.2015.01.011 | sci-hub.la/10.1016/j.ijpsycho.2015.01.011 | 10.1016/j.ijpsycho.2015.01.011 | - | |||
| Reinforcement learning in depression: A review of computational research. | 2015 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/25979140 | sci-hub.tw/10.1016/j.neubiorev.2015.05.005 | sci-hub.la/10.1016/j.neubiorev.2015.05.005 | 10.1016/j.neubiorev.2015.05.005 | - | |||
| Role of the Brain's Reward Circuitry in Depression: Transcriptional Mechanisms. | 2015 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/26472529 | sci-hub.tw/10.1016/bs.irn.2015.07.003 | sci-hub.la/10.1016/bs.irn.2015.07.003 | 10.1016/bs.irn.2015.07.003 | - | |||
| The serotonin transporter in depression: Meta-analysis of in vivo and post mortem findings and implications for understanding and treating depression. | 2015 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/26281039 | sci-hub.tw/10.1016/j.jad.2015.07.034 | sci-hub.la/10.1016/j.jad.2015.07.034 | 10.1016/j.jad.2015.07.034 | - | |||
| The Brain's Response to Reward Anticipation and Depression in Adolescence: Dimensionality, Specificity, and Longitudinal Predictions in a Community-Based Sample. | 2015 | MDD | 1 | 1576 | https://www.ncbi.nlm.nih.gov/pubmed/26085042 | sci-hub.tw/10.1176/appi.ajp.2015.14101298 | sci-hub.la/10.1176/appi.ajp.2015.14101298 | 10.1176/appi.ajp.2015.14101298 | 1576.0 | |||
| Large-Scale Network Dysfunction in Major Depressive Disorder: A Meta-analysis of Resting-State Functional Connectivity. | 2015 | MDD | 27 | 1074 | https://www.ncbi.nlm.nih.gov/pubmed/25785575 | sci-hub.tw/10.1001/jamapsychiatry.2015.0071 | sci-hub.la/10.1001/jamapsychiatry.2015.0071 | 10.1001/jamapsychiatry.2015.0071 | 39.8 | |||
| Voxel-wise meta-analyses of brain blood flow and local synchrony abnormalities in medication-free patients with major depressive disorder. | 2015 | MDD | 23 | 1068 | https://www.ncbi.nlm.nih.gov/pubmed/25853283 | sci-hub.tw/10.1503/jpn.140119 | sci-hub.la/10.1503/jpn.140119 | 10.1503/jpn.140119 | 46.4 | |||
| Neuropsychological mechanism underlying antidepressant effect: a systematic meta-analysis | 2015 | MDD | 50 | 1569 | https://www.ncbi.nlm.nih.gov/pubmed/24662929 | sci-hub.tw/10.1038/mp.2014.24 | sci-hub.la/10.1038/mp.2014.24 | 10.1038/mp.2014.24 | 31.4 | |||
| Molecular imaging of striatal dopamine transporters in major depression--a meta-analysis. | 2015 | MDD | 12 | 523 | https://www.ncbi.nlm.nih.gov/pubmed/25497470 | sci-hub.tw/10.1016/j.jad.2014.11.045 | sci-hub.la/10.1016/j.jad.2014.11.045 | 10.1016/j.jad.2014.11.045 | 43.6 | |||
| Meta-analysis of Functional Neuroimaging of Major Depressive Disorder in Youth. | 2015 | MDD | 14 | 520 | https://www.ncbi.nlm.nih.gov/pubmed/26332700 | sci-hub.tw/10.1001/jamapsychiatry.2015.1376 | sci-hub.la/10.1001/jamapsychiatry.2015.1376 | 10.1001/jamapsychiatry.2015.1376 | 37.1 | |||
| Optogenetics to study the circuits of fear- and depression-like behaviors: a critical analysis. | 2014 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/24727401 | sci-hub.tw/10.1016/j.pbb.2014.04.002 | sci-hub.la/10.1016/j.pbb.2014.04.002 | 10.1016/j.pbb.2014.04.002 | - | |||
| Deep brain stimulation of the human reward system for major depression--rationale, outcomes and outlook. | 2014 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/24513970 | sci-hub.tw/10.1038/npp.2014.28 | sci-hub.la/10.1038/npp.2014.28 | 10.1038/npp.2014.28 | - | |||
| Meta-analysis of molecular imaging of serotonin transporters in major depression. | 2014 | MDD | 18 | 736 | https://www.ncbi.nlm.nih.gov/pubmed/24802331 | sci-hub.tw/10.1038/jcbfm.2014.82 | sci-hub.la/10.1038/jcbfm.2014.82 | 10.1038/jcbfm.2014.82 | 40.9 | |||
| Optogenetic dissection of neural circuits underlying emotional valence and motivated behaviors. | 2013 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/23142759 | sci-hub.tw/10.1016/j.brainres.2012.11.001 | sci-hub.la/10.1016/j.brainres.2012.11.001 | 10.1016/j.brainres.2012.11.001 | - | |||
| The brain reward circuitry in mood disorders. | 2013 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/23942470 | sci-hub.tw/10.1038/nrn3381 | sci-hub.la/10.1038/nrn3381 | 10.1038/nrn3381 | - | |||
| Neuroreceptor imaging in depression. | 2013 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/22691454 | sci-hub.tw/10.1016/j.nbd.2012.06.001 | sci-hub.la/10.1016/j.nbd.2012.06.001 | 10.1016/j.nbd.2012.06.001 | - | |||
| Gray matter volume in major depressive disorder: a meta-analysis of voxel-based morphometry studies. | 2013 | MDD | 20 | 1594 | https://www.ncbi.nlm.nih.gov/pubmed/23146253 | sci-hub.tw/10.1016/j.pscychresns.2012.06.006 | sci-hub.la/10.1016/j.pscychresns.2012.06.006 | 10.1016/j.pscychresns.2012.06.006 | 79.7 | |||
| Meta-analytic evidence for neuroimaging models of depression: state or trait? | 2013 | MDD | 40 | 1270 | https://www.ncbi.nlm.nih.gov/pubmed/23890584 | sci-hub.tw/10.1016/j.jad.2013.07.002 | sci-hub.la/10.1016/j.jad.2013.07.002 | 10.1016/j.jad.2013.07.002 | 31.8 | |||
| Resting-state brain activity in schizophrenia and major depression: a quantitative meta-analysis. | 2013 | MDD | 11 | 470 | https://www.ncbi.nlm.nih.gov/pubmed/22080493 | sci-hub.tw/10.1093/schbul/sbr151 | sci-hub.la/10.1093/schbul/sbr151 | 10.1093/schbul/sbr151 | 42.7 | |||
| A meta-analysis of neurofunctional imaging studies of emotion and cognition in major depression. | 2012 | MDD | 40 | 1127 | https://www.ncbi.nlm.nih.gov/pubmed/22521254 | sci-hub.tw/10.1016/j.neuroimage.2012.04.005 | sci-hub.la/10.1016/j.neuroimage.2012.04.005 | 10.1016/j.neuroimage.2012.04.005 | 28.2 | |||
| Functional neuroimaging of major depressive disorder: a meta-analysis and new integration of base line activation and neural response data. | 2012 | MDD | 14 | 599 | https://www.ncbi.nlm.nih.gov/pubmed/22535198 | sci-hub.tw/10.1176/appi.ajp.2012.11071105 | sci-hub.la/10.1176/appi.ajp.2012.11071105 | 10.1176/appi.ajp.2012.11071105 | 42.8 | |||
| Structural and functional neuroimaging studies of the suicidal brain. | 2011 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/21216267 | sci-hub.tw/10.1016/j.pnpbp.2010.12.026 | sci-hub.la/10.1016/j.pnpbp.2010.12.026 | 10.1016/j.pnpbp.2010.12.026 | - | |||
| Structural neuroimaging studies in major depressive disorder. Meta-analysis and comparison with bipolar disorder. | 2011 | MDD | 143 | 18379 | https://www.ncbi.nlm.nih.gov/pubmed/21727252 | sci-hub.tw/10.1001/archgenpsychiatry.2011.60 | sci-hub.la/10.1001/archgenpsychiatry.2011.60 | 10.1001/archgenpsychiatry.2011.60 | 128.5 | |||
| Functional neuroimaging of reward processing and decision-making: a review of aberrant motivational and affective processing in addiction and mood disorders. | 2008 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/18675846 | sci-hub.tw/10.1016/j.brainresrev.2008.07.004 | sci-hub.la/10.1016/j.brainresrev.2008.07.004 | 10.1016/j.brainresrev.2008.07.004 | - | |||
| Dynamics of the dopaminergic system as a key component to the understanding of depression. | 2008 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/18772037 | sci-hub.tw/10.1016/S0079-6123(08)00913-8 | sci-hub.la/10.1016/S0079-6123(08)00913-8 | 10.1016/S0079-6123(08)00913-8 | - | |||
| The mesolimbic dopamine reward circuit in depression. | 2006 | MDD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/16566899 | sci-hub.tw/10.1016/j.biopsych.2005.09.018 | sci-hub.la/10.1016/j.biopsych.2005.09.018 | 10.1016/j.biopsych.2005.09.018 | - | |||
| Review of 1H magnetic resonance spectroscopy findings in major depressive disorder: a meta-analysis. | 2006 | MDD | 42 | 1688 | https://www.ncbi.nlm.nih.gov/pubmed/16806850 | sci-hub.tw/10.1016/j.pscychresns.2005.12.004 | sci-hub.la/10.1016/j.pscychresns.2005.12.004 | 10.1016/j.pscychresns.2005.12.004 | 40.2 | |||
| Distinct Subcortical Volume Alterations in Pediatric and Adult OCD: A Worldwide Meta- and Mega-Analysis. | 2017 | OCD | 1 | 3589 | https://www.ncbi.nlm.nih.gov/pubmed/27609241 | sci-hub.tw/10.1176/appi.ajp.2016.16020201 | sci-hub.la/10.1176/appi.ajp.2016.16020201 | 10.1176/appi.ajp.2016.16020201 | 3589.0 | |||
| Neural correlates of affective and non-affective cognition in obsessive compulsive disorder: A meta-analysis of functional imaging studies. | 2017 | OCD | 54 | 2345 | https://www.ncbi.nlm.nih.gov/pubmed/28992533 | sci-hub.tw/10.1016/j.eurpsy.2017.08.001 | sci-hub.la/10.1016/j.eurpsy.2017.08.001 | 10.1016/j.eurpsy.2017.08.001 | 43.4 | |||
| Meta-analytic investigations of common and distinct grey matter alterations in youths and adults with obsessive-compulsive disorder. | 2017 | OCD | 25 | 1575 | https://www.ncbi.nlm.nih.gov/pubmed/28442404 | sci-hub.tw/10.1016/j.neubiorev.2017.04.012 | sci-hub.la/10.1016/j.neubiorev.2017.04.012 | 10.1016/j.neubiorev.2017.04.012 | 63.0 | |||
| Structural and Functional Brain Abnormalities in Attention-Deficit/Hyperactivity Disorder and Obsessive-Compulsive Disorder: A Comparative Meta-analysis. | 2016 | OCD | 108 | 5274 | https://www.ncbi.nlm.nih.gov/pubmed/27276220 | sci-hub.tw/10.1001/jamapsychiatry.2016.0700 | sci-hub.la/10.1001/jamapsychiatry.2016.0700 | 10.1001/jamapsychiatry.2016.0700 | 48.8 | |||
| Meta-analytic investigations of structural grey matter, executive domain-related functional activations, and white matter diffusivity in obsessive compulsive disorder: an integrative review. | 2015 | OCD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/25766413 | sci-hub.tw/10.1016/j.neubiorev.2015.03.002 | sci-hub.la/10.1016/j.neubiorev.2015.03.002 | 10.1016/j.neubiorev.2015.03.002 | - | |||
| Multimodal voxel-based meta-analysis of white matter abnormalities in obsessive-compulsive disorder. | 2015 | OCD | 22 | 1112 | https://www.ncbi.nlm.nih.gov/pubmed/24407265 | sci-hub.tw/10.1038/npp.2014.5 | sci-hub.la/10.1038/npp.2014.5 | 10.1038/npp.2014.5 | 50.5 | |||
| Brain circuitries of obsessive compulsive disorder: a systematic review and meta-analysis of diffusion tensor imaging studies. | 2013 | OCD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/24177038 | sci-hub.tw/10.1016/j.neubiorev.2013.10.008 | sci-hub.la/10.1016/j.neubiorev.2013.10.008 | 10.1016/j.neubiorev.2013.10.008 | - | |||
| Neuroimaging of cognitive brain function in paediatric obsessive compulsive disorder: a review of literature and preliminary meta-analysis. | 2012 | OCD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/22678698 | sci-hub.tw/10.1007/s00702-012-0813-z | sci-hub.la/10.1007/s00702-012-0813-z | 10.1007/s00702-012-0813-z | - | |||
| Reduction of N-acetylaspartate in the medial prefrontal cortex correlated with symptom severity in obsessive-compulsive disorder: meta-analyses of (1)H-MRS studies. | 2012 | OCD | 16 | 458 | https://www.ncbi.nlm.nih.gov/pubmed/22892718 | sci-hub.tw/10.1038/tp.2012.78 | sci-hub.la/10.1038/tp.2012.78 | 10.1038/tp.2012.78 | 28.6 | |||
| Gray matter alterations in obsessive-compulsive disorder: an anatomic likelihood estimation meta-analysis. | 2010 | OCD | 10 | 661 | https://www.ncbi.nlm.nih.gov/pubmed/19890260 | sci-hub.tw/10.1038/npp.2009.175 | sci-hub.la/10.1038/npp.2009.175 | 10.1038/npp.2009.175 | 66.1 | |||
| Meta-analysis of brain volume changes in obsessive-compulsive disorder. | 2009 | OCD | 14 | 778 | https://www.ncbi.nlm.nih.gov/pubmed/18718575 | sci-hub.tw/10.1016/j.biopsych.2008.06.019 | sci-hub.la/10.1016/j.biopsych.2008.06.019 | 10.1016/j.biopsych.2008.06.019 | 55.6 | |||
| Voxel-wise meta-analysis of grey matter changes in obsessive-compulsive disorder. | 2009 | OCD | 12 | 777 | https://www.ncbi.nlm.nih.gov/pubmed/19880927 | sci-hub.tw/10.1192/bjp.bp.108.055046 | sci-hub.la/10.1192/bjp.bp.108.055046 | 10.1192/bjp.bp.108.055046 | 64.8 | |||
| Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: the orbitofronto-striatal model revisited. | 2008 | OCD | - | - | https://www.ncbi.nlm.nih.gov/pubmed/18061263 | sci-hub.tw/10.1016/j.neubiorev.2007.09.005 | sci-hub.la/10.1016/j.neubiorev.2007.09.005 | 10.1016/j.neubiorev.2007.09.005 | - | |||
| Provocation of obsessive–compulsive symptoms: a quantitative voxel-based meta-analysis of functional neuroimaging studies | 2008 | OCD | 8 | 94 | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2527721/ | sci-hub.tw/https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2527721/ | sci-hub.la/https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2527721/ | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2527721/ | 11.8 | |||
| A meta-analysis of functional neuroimaging in obsessive-compulsive disorder. | 2004 | OCD | 13 | 40 | https://www.ncbi.nlm.nih.gov/pubmed/15546704 | sci-hub.tw/10.1016/j.pscychresns.2004.07.001 | sci-hub.la/10.1016/j.pscychresns.2004.07.001 | 10.1016/j.pscychresns.2004.07.001 | 3.1 | |||
| Different patterns of 5-HT receptor and transporter dysfunction in neuropsychiatric disorders--a comparative analysis of in vivo imaging findings. | 2016 | PSY | 136 | - | https://www.ncbi.nlm.nih.gov/pubmed/26376220 | sci-hub.tw/10.1515/revneuro-2015-0014 | sci-hub.la/10.1515/revneuro-2015-0014 | 10.1515/revneuro-2015-0014 | - | |||
| Mapping anhedonia-specific dysfunction in a transdiagnostic approach: an ALE meta-analysis. | 2016 | PSY | 89 | 3272 | https://www.ncbi.nlm.nih.gov/pubmed/26487590 | sci-hub.tw/10.1007/s11682-015-9457-6 | sci-hub.la/10.1007/s11682-015-9457-6 | 10.1007/s11682-015-9457-6 | 36.8 | |||
| The serotonin transporter in psychiatric disorders: insights from PET imaging. | 2015 | PSY | - | - | https://www.ncbi.nlm.nih.gov/pubmed/26249305 | sci-hub.tw/10.1016/S2215-0366(15)00232-1 | sci-hub.la/10.1016/S2215-0366(15)00232-1 | 10.1016/S2215-0366(15)00232-1 | - | |||
| Mechanisms Underlying Motivational Deficits in Psychopathology: Similarities and Differences in Depression and Schizophrenia. | 2014 | PSY | - | - | https://www.ncbi.nlm.nih.gov/pubmed/26026289 | sci-hub.tw/10.1007/7854_2015_376 | sci-hub.la/10.1007/7854_2015_376 | 10.1007/7854_2015_376 | - | |||
| Brain imaging findings in children and adolescents with mental disorders: a cross-sectional review | 2010 | PSY | 274 | - | https://www.ncbi.nlm.nih.gov/pubmed/20620025 | sci-hub.tw/10.1016/j.eurpsy.2010.04.010 | sci-hub.la/10.1016/j.eurpsy.2010.04.010 | 10.1016/j.eurpsy.2010.04.010 | - | |||
| The IMAGEN study: reinforcement-related behaviour in normal brain function and psychopathology. | 2010 | PSY | - | - | https://www.ncbi.nlm.nih.gov/pubmed/21102431 | sci-hub.tw/10.1038/mp.2010.4 | sci-hub.la/10.1038/mp.2010.4 | 10.1038/mp.2010.4 | - | |||
| Aberrant Resting-State Brain Activity in Post-Traumatic Stress Disorder: A Meta-Analysis And Systematic Review. | 2016 | PTSD | 23 | 663 | https://www.ncbi.nlm.nih.gov/pubmed/26918313 | sci-hub.tw/10.1002/da.22478 | sci-hub.la/10.1002/da.22478 | 10.1002/da.22478 | 28.8 | |||
| In search of the trauma memory: a meta-analysis of functional neuroimaging studies of symptom provocation in posttraumatic stress disorder (PTSD). | 2013 | PTSD | 14 | 66 | https://www.ncbi.nlm.nih.gov/pubmed/23536785 | sci-hub.tw/10.1371/journal.pone.0058150 | sci-hub.la/10.1371/journal.pone.0058150 | 10.1371/journal.pone.0058150 | 4.7 | |||
| Common and distinct neural correlates of facial emotion processing in social anxiety disorder and Williams syndrome: A systematic review and voxel-based meta-analysis of functional resonance imaging studies. | 2014 | SAD | 17 | 575 | https://www.ncbi.nlm.nih.gov/pubmed/25194208 | sci-hub.tw/10.1016/j.neuropsychologia.2014.08.027 | sci-hub.la/10.1016/j.neuropsychologia.2014.08.027 | 10.1016/j.neuropsychologia.2014.08.027 | 33.8 | |||
| Neuroimaging in social anxiety disorder—a meta-analytic review resulting in a new neurofunctional model. | 2014 | SAD | 19 | 409 | https://www.ncbi.nlm.nih.gov/pubmed/25124509 | sci-hub.tw/10.1016/j.neubiorev.2014.08.003 | sci-hub.la/10.1016/j.neubiorev.2014.08.003 | 10.1016/j.neubiorev.2014.08.003 | 21.5 | |||
| Schizophrenia symptomatic associations with diffusion tensor imaging measured fractional anisotropy of brain: a meta-analysis. | 2017 | SCZ | 33 | 2242 | https://www.ncbi.nlm.nih.gov/pubmed/28550466 | sci-hub.tw/10.1007/s00234-017-1844-9 | sci-hub.la/10.1007/s00234-017-1844-9 | 10.1007/s00234-017-1844-9 | 67.9 | |||
| Positive symptoms associate with cortical thinning in the superior temporal gyrus via the ENIGMA Schizophrenia consortium. | 2017 | SCZ | 1 | 1987 | https://www.ncbi.nlm.nih.gov/pubmed/28369804 | sci-hub.tw/10.1111/acps.12718 | sci-hub.la/10.1111/acps.12718 | 10.1111/acps.12718 | 1987.0 | |||
| Patients with schizophrenia show aberrant patterns of basal ganglia activation: Evidence from ALE meta-analysis. | 2017 | SCZ | 42 | 1290 | https://www.ncbi.nlm.nih.gov/pubmed/28275545 | sci-hub.tw/10.1016/j.nicl.2017.01.034 | sci-hub.la/10.1016/j.nicl.2017.01.034 | 10.1016/j.nicl.2017.01.034 | 30.7 | |||
| Brain-Wide Analysis of Functional Connectivity in First-Episode and Chronic Stages of Schizophrenia. | 2017 | SCZ | 6 | 789 | https://www.ncbi.nlm.nih.gov/pubmed/27445261 | sci-hub.tw/10.1093/schbul/sbw099 | sci-hub.la/10.1093/schbul/sbw099 | 10.1093/schbul/sbw099 | 131.5 | |||
| Altered Hub Functioning and Compensatory Activations in the Connectome: A Meta-Analysis of Functional Neuroimaging Studies in Schizophrenia. | 2016 | SCZ | 314 | 10000 | https://www.ncbi.nlm.nih.gov/pubmed/26472684 | sci-hub.tw/10.1093/schbul/sbv146 | sci-hub.la/10.1093/schbul/sbv146 | 10.1093/schbul/sbv146 | 31.8 | |||
| The neural mechanisms of hallucinations: A quantitative meta-analysis of neuroimaging studies. | 2016 | SCZ | 17 | 211 | https://www.ncbi.nlm.nih.gov/pubmed/27473935 | sci-hub.tw/10.1016/j.neubiorev.2016.05.037 | sci-hub.la/10.1016/j.neubiorev.2016.05.037 | 10.1016/j.neubiorev.2016.05.037 | 12.4 | |||
| Rostral medial prefrontal dysfunctions and consummatory pleasure in schizophrenia: a meta-analysis of functional imaging studies. | 2015 | SCZ | 19 | 615 | https://www.ncbi.nlm.nih.gov/pubmed/25637357 | sci-hub.tw/10.1016/j.pscychresns.2015.01.001 | sci-hub.la/10.1016/j.pscychresns.2015.01.001 | 10.1016/j.pscychresns.2015.01.001 | 32.4 | |||
| Alterations in the serotonin system in schizophrenia: a systematic review and meta-analysis of postmortem and molecular imaging studies. | 2014 | SCZ | - | - | https://www.ncbi.nlm.nih.gov/pubmed/24971825 | sci-hub.tw/10.1016/j.neubiorev.2014.06.005 | sci-hub.la/10.1016/j.neubiorev.2014.06.005 | 10.1016/j.neubiorev.2014.06.005 | - | |||
| Alterations in cortical and extrastriatal subcortical dopamine function in schizophrenia: systematic review and meta-analysis of imaging studies. | 2014 | SCZ | 23 | 543 | https://www.ncbi.nlm.nih.gov/pubmed/25029687 | sci-hub.tw/10.1192/bjp.bp.113.132308 | sci-hub.la/10.1192/bjp.bp.113.132308 | 10.1192/bjp.bp.113.132308 | 23.6 | |||
| Brain vs behavior: an effect size comparison of neuroimaging and cognitive studies of genetic risk for schizophrenia. | 2013 | SCZ | - | - | https://www.ncbi.nlm.nih.gov/pubmed/22499782 | sci-hub.tw/10.1093/schbul/sbs056 | sci-hub.la/10.1093/schbul/sbs056 | 10.1093/schbul/sbs056 | - | |||
| Striatal presynaptic dopamine in schizophrenia, Part I: meta-analysis of dopamine active transporter (DAT) density. | 2013 | SCZ | 13 | 349 | https://www.ncbi.nlm.nih.gov/pubmed/22282456 | sci-hub.tw/10.1093/schbul/sbr111 | sci-hub.la/10.1093/schbul/sbr111 | 10.1093/schbul/sbr111 | 26.8 | |||
| Striatal presynaptic dopamine in schizophrenia, part II: meta-analysis of [(18)F/(11)C]-DOPA PET studies. | 2013 | SCZ | 11 | 244 | https://www.ncbi.nlm.nih.gov/pubmed/22282454 | sci-hub.tw/10.1093/schbul/sbr180 | sci-hub.la/10.1093/schbul/sbr180 | 10.1093/schbul/sbr180 | 22.2 | |||
| Meta-analysis of functional neuroimaging studies of emotion perception and experience in schizophrenia. | 2012 | SCZ | 26 | 872 | https://www.ncbi.nlm.nih.gov/pubmed/21993193 | sci-hub.tw/10.1016/j.biopsych.2011.09.007 | sci-hub.la/10.1016/j.biopsych.2011.09.007 | 10.1016/j.biopsych.2011.09.007 | 33.5 | |||
| Quantitative meta-analysis on state and trait aspects of auditory verbal hallucinations in schizophrenia. | 2012 | SCZ | 15 | 274 | https://www.ncbi.nlm.nih.gov/pubmed/21177743 | sci-hub.tw/10.1093/schbul/sbq152 | sci-hub.la/10.1093/schbul/sbq152 | 10.1093/schbul/sbq152 | 18.3 | |||
| The "paradoxical" engagement of the primary auditory cortex in patients with auditory verbal hallucinations: a meta-analysis of functional neuroimaging studies. | 2011 | SCZ | 12 | 477 | https://www.ncbi.nlm.nih.gov/pubmed/21872614 | sci-hub.tw/10.1016/j.neuropsychologia.2011.08.010 | sci-hub.la/10.1016/j.neuropsychologia.2011.08.010 | 10.1016/j.neuropsychologia.2011.08.010 | 39.8 | |||
| Facial emotion processing in schizophrenia: a meta-analysis of functional neuroimaging data. | 2010 | SCZ | 17 | - | https://www.ncbi.nlm.nih.gov/pubmed/19336391 | sci-hub.tw/10.1093/schbul/sbn190 | sci-hub.la/10.1093/schbul/sbn190 | 10.1093/schbul/sbn190 | - | |||
| Meta-analysis of 41 functional neuroimaging studies of executive function in schizophrenia. | 2009 | SCZ | 41 | - | https://www.ncbi.nlm.nih.gov/pubmed/19652121 | sci-hub.tw/10.1001/archgenpsychiatry.2009.91 | sci-hub.la/10.1001/archgenpsychiatry.2009.91 | 10.1001/archgenpsychiatry.2009.91 | - | |||
| Neural correlates of somatoform disorders from a meta-analytic perspective on neuroimaging studies. | 2016 | SD | 10 | 447 | https://www.ncbi.nlm.nih.gov/pubmed/27182487 | sci-hub.tw/10.1016/j.nicl.2016.04.001 | sci-hub.la/10.1016/j.nicl.2016.04.001 | 10.1016/j.nicl.2016.04.001 | 44.7 | |||
| Neural correlates of conversion disorder: overview and meta-analysis of neuroimaging studies on motor conversion disorder. | 2016 | SD | 12 | 335 | https://www.ncbi.nlm.nih.gov/pubmed/27283002 | sci-hub.tw/10.1186/s12888-016-0890-x | sci-hub.la/10.1186/s12888-016-0890-x | 10.1186/s12888-016-0890-x | 27.9 |
| Title | Summary | Pubmed |
|---|---|---|
| Melancholy, anhedonia, apathy: the search for separable behaviors and neural circuits in depression. | In rodent models of depression, activity in the mPFC as a whole relates to reduced sucrose preference and sociability, with are thought to be analogous to anhedonia and social withdrawal, respectively, in humans. Inhibiting this region via stimulating it at a supraphysiological frequency appears to attenuate these deficits. | https://www.ncbi.nlm.nih.gov/pubmed/29529482 |
| Circuit-based frameworks of depressive behaviors: The role of reward circuitry and beyond. | Evidence related to the role of the VTA in producing depression-like behaviors in animals is complex. | https://www.ncbi.nlm.nih.gov/pubmed/29309799 |
| Treatment resistant depression: A multi-scale, systems biology approach. | https://www.ncbi.nlm.nih.gov/pubmed/28859997 | |
| Dopamine System Dysregulation in Major Depressive Disorders. | A | https://www.ncbi.nlm.nih.gov/pubmed/29106542 |
| Progress in understanding mood disorders: optogenetic dissection of neural circuits. | A | https://www.ncbi.nlm.nih.gov/pubmed/23682971 |
| Presentation and Neurobiology of Anhedonia in Mood Disorders: Commonalities and Distinctions. | A | https://www.ncbi.nlm.nih.gov/pubmed/29520717 |
| Neuroimaging genomic studies in major depressive disorder: A systematic review. | A | https://www.ncbi.nlm.nih.gov/pubmed/29476595 |
| Lateral habenula in the pathophysiology of depression. | A | https://www.ncbi.nlm.nih.gov/pubmed/29175713 |
| Intrinsic cerebral activity at resting state in adults with major depressive disorder: A meta-analysis. | A | https://www.ncbi.nlm.nih.gov/pubmed/28174129 |
| Characterization of brain blood flow and the amplitude of low-frequency fluctuations in major depressive disorder: A multimodal meta-analysis. | A | https://www.ncbi.nlm.nih.gov/pubmed/28068619 |
| Altered Brain Activity in Unipolar Depression Revisited: Meta-analyses of Neuroimaging Studies. | A | https://www.ncbi.nlm.nih.gov/pubmed/27829086 |
Pathophysiology of PTSD
Anhedonia
VTA
- The heterogeneity of ventral tegmental area neurons: Projection functions in a mood-related context
- Reward and aversion in a heterogeneous midbrain dopamine system
- Medial VTA DA neurons project to the medial shell of the NAc as well as the NAc core, the mPFC and the BLA. Lateral VTA DA neurons project to the lateral NAc shell, and likely represent the population of neurons that were historically assessed in studies that identified DA neurons by waveform and electrophysiological characteristics.
- The LDTg projects to the lVTA, driving the lVTA to release DA in the lateral NAc shell, producing CPP. The LHb, on the other hand, excites RMTg neurons that inhibit lVTA-Lateral NAc shell projections, but also excites NAc-->mPFC projections, inducing CPA.
- The antero-posterior heterogeneity of the ventral tegmental area
- Dopamine and reward seeking: the role of ventral tegmental area
- Circuit-based frameworks of depressive behaviors: The role of reward circuitry and beyond
- Opioid and hypocretin neuromodulation of ventral tegmental area neuronal subpopulations
- Lateral Hypothalamic Control of the Ventral Tegmental Area: Reward Evaluation and the Driving of Motivated Behavior.
- Organization of dopamine and serotonin system: Anatomical and functional mapping of monosynaptic inputs using rabies virus
- The VTA receives input from the lOFC, ventral striatum, BNST, ventral pallidum, lateral hypothalamus, PPTg, and central nucleus of the amygdala. These areas encode a distributed representation of reward expectation and outcome with a high degree of redundancy.
- The DR sends glutaminergic projections to the VTA which drive incentive salience; the LHb sends glutaminergic projections to the RMTg and mVTA to mPFC projections, the former of which provides general inhibition to DAergic neurons, and the latter of which excited mVTA to mPFC projections producing aversion; the BNST sends glutaminergic projections to GABAergic neurons, driving aversion, and GABAergic projections to GABAergic neurons, driving reward; the LH sends a pattern of projections similar to the BNST; the LDTg sends reward driving glutaminergic and GABAergic/glutaminergic coreleasing inputs to the VTA.
- Supports similar results as with (Cardozo Pinto and Lammel), but also includes VTA--->NAc PV---|NAc producing aversion
- Input-specific contributions to valence processing in the amygdala.
- Ventral tegmental area subcircuits process rewarding and aversive experiences.
- Dopamine reward prediction error coding
- Ventral Tegmental Area Afferents and Drug-Dependent Behaviors.
- Neurophysiology of Reward-Guided Behavior: Correlates Related to Predictions, Value, Motivation, Errors, Attention, and Action
- OFC inputs to the VTA are necessary for error signals.
Recent
- Role of Protein Kinase C in Bipolar Disorder: A Review of the Current Literature
- The search for neuroimaging and cognitive endophenotypes: A critical systematic review of studies involving unaffected first-degree relatives of individuals with bipolar disorder
- Assessing the role of cingulate cortex in bipolar disorder: neuropathological, structural and functional imaging data.
- Neurobiological evidence for thalamic, hippocampal and related glutamatergic abnormalities in bipolar disorder: a review and synthesis.
- Neuropsychological underpinnings of the dynamics of bipolar disorder.
- Variants in Ion Channel Genes Link Phenotypic Features of Bipolar Illness to Specific Neurobiological Process Domains
- New insights help define the pathophysiology of bipolar affective disorder: neuroimaging and neuropathology findings
Schizophrenia
The cause and mechanism of schizophrenia is unknown. Evidence from phenomenology, pharmacology, neuroimaging, post mortem studies, genetics, and animal models implicate a number of possible and likely interrelated mechanisms, such as abnormalities in dopaminergic signalling, glutaminergic neurotransmission, and neurodevelopment. Many frameworks have been hypothesized to link these biological abnormalities to symptoms, including psychological and computational theories.[52][53]
Abnormal dopamine signalling has been implicated in schizophrenia by the efficacy of D2 receptor antagonists, as well as the consistent observation in positron emission tomography of elevated dopamine synthesis[54] and release during acute psychosis.[55] Abnormalities in dopaminergic symptoms have been hypothesized to underlie delusions via dysfunctional signalling of salience.[56][57][58] Dopaminergic predictions errors, which mediate learning when expectancies are violated, are abnormal in schizophrenia, and these abnormalities correlate with the severity of delusions. Furthermore, impaired learning, putatively reflecting the functionality of the dopaminergic system, is present in schizophrenia and correlates with delusion severity.[59] Dysfunctional prediction errors may be related to hyperactive input from the hippocampus, which is observed to be metabolically overactive in schizophrenia,[56] and in turn may be related to abnormalities in NMDA receptor functioning on hippocampal interneurons.[60] Hypoactivation of D1 receptors in the prefrontal cortex may also be responsible for deficits in working memory and cognition,[61][62][63][64] although direct evidence from neuroreceptor imaging studies is inconsistent.[65]
Reduced NMDA receptor signalling is suggested by multiple lines of evidence. Post-mortem studies demonstrate reduced NMDA receptor expression and NMDA receptor antagonists mimic both schizophrenia symptoms and the electrophysiological abnormalities associated with schizophrenia (notable reduced mismatch negativity and P300).[66][67][68] Two meta analyses of magnetic resonance spectroscopy studies have found evidence interpreted to be consistent with abnormal glutaminergic signalling, possible involving NMDA receptor abnormalities, despite contradictory findings (i.e. reduced versus elevated glutamate/glutamine ratios).[69][70] This deficit in NMDA signalling may be related to the abnormalities observed in parvalbumin interneurons that express NMDA receptors.[71] Post mortem studies consistently find that a subset of these neurons fail to express GAD67 in addition to abnormalities in morphology,[72] although neuroimaging studies examining indicators of GABAergic signalling do not consistently report abnormalities.[73][74] The subsets of interneurons that are abnormal in schizophrenia are responsible for the synchronizing of neural ensembles that is necessary during working memory tasks, a process that is electrophysiologically reflected in gamma frequency (30-80 Hz) oscillations. Both working memory tasks and gamma oscillations are impaired in schizophrenia, which may reflect abnormal interneuron functionality.[75][76][77][78][79]
Multiple lines of evidence suggest that schizophrenia has a neurodevelopmental component.[80] Schizophrenia is associated with premorbid impairments in cognition, social functioning, and motor skills,[81] and prenatal insults such as maternal infection,[82][83] maternal malnutrition and obsteric complications all increase risk for schizophrenia.[84] Animal models of these insults demonstrate patterns of cellular and molecular abnormalities similar to those in schizophrenia, such as increased RELN methylation and abnormal GABAergic cell development.[85] Schizophrenia usually emerges symptomatically during late adolescence, 18-25, an age period that overlaps with certain stages of neurodevelopment that are implicated in schizophrenia, such as abnormal synaptic pruning and myelination.[86]
Deficits in executive functions, such as planning, inhibition, and working memory, are pervasive in schizophrenia. Although these functions are dissociable, their dysfunction in schizophrenia may reflect an underlying deficit in the ability to represent goal related information in working memory, and to utilize this to direct cognition and behavior.[87][88] These impairments have been linked to a number of neuroimaging and neuropathological abnormalities. For example, functional neuroimaging studies report evidence of reduced neural processing efficiency, whereby the dorsolateral prefrontal cortex is activated to a greater degree to achieve a certain level of performance relative to controls on working memory tasks. These abnormalities may be linked to the consistent post-mortem finding of reduced neuropil, evidenced by increased pyramidal cell density, reduced dentritic spine density,[89] and reduced expression mRNA associated with synapses.[90] These cellular and functional abnormalities may also be reflected in structural neuroimaging studies that find reduced grey matter volume in association with deficits in working memory tasks.[89]
Different symptoms have been linked to specific neuroanatomical abnormalities or neurobiological models. For example, positive and negative symptoms have been linked to reduced cortical thickness in the superior temporal lobe,[91] and orbitofrontal cortex, respectively.[92] Auditory hallucinations, a prominent component of positive symptoms, are also reflected in functional hyperactivity of auditory cortices, and in the predictive coding framework are hypothesized to reflect impaired feedforward cancellation of internally generated speech.[93] Anhedonia, traditionally defined as a reduced capacity to experience pleasure, is frequently reported in schizophrenia. However, a large body of evidence suggests that hedonic responses are intact in schizophrenia,[94] and that what is reported to be anhedonia is a reflection of dysfunction in other processes related to reward.[95] Overall, a failure of online maintenance and reward associativity is thought to lead to impairment in the generation of cognition and behavior required to obtain rewards, despite normal hedonic responses.[96] A meta analysis of neuroimaging studies examining reward related paradigms reported results consistent with impairments in the neural substrates that mediate learning, but not in the experience of reward.[97]
Bayesian models of brain function have been utilized to link abnormalities in cellular functioning to symptoms. These models propose that the brain generates predictive models in order to explain sensory information, and that predictive units are organized in a hierarchical fashion that reflect a more abstract model of causes for sensory information higher in the hierarchy. The essential computation performed by these models involves the minimization of error generated by discrepancies in top down predictions by modifying synaptic weights with the least precision.[98][99] Improper specification of precision in bayesian models is largely consistent with the behavioral, neuroimaging, and electrophysiological abnormalities associated with schizophrenia. Both a failure to attenuate sensory precision and excessive weighting or priors have been proposed as potential and not necessarily conflicting explanations.[100] In canonical models of circuits that mediate predictive coding, hypoactive NMDA receptor activation and abnormalities in dopaminergic signalling,[101] similar to that seen in schizophrenia, could theoretically result in classic symptoms of schizophrenia such as delusions and hallucinations.[102][59][103]
Images



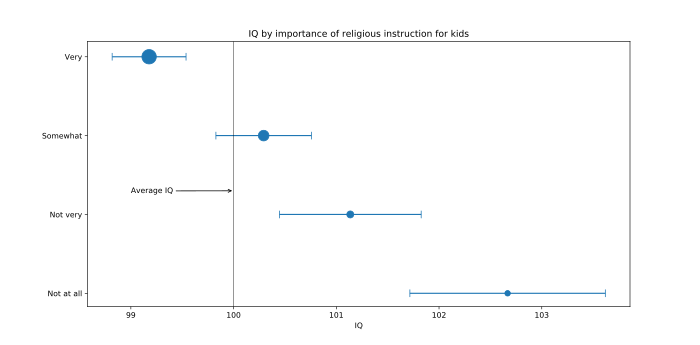
OLS Regression Results
==============================================================================
Dep. Variable: g factor R-squared: 0.202
Model: OLS Adj. R-squared: 0.201
Method: Least Squares F-statistic: 293.2
Date: Thu, 02 Aug 2018 Prob (F-statistic): 1.11e-169
Time: 12:11:03 Log-Likelihood: -4542.1
No. Observations: 3478 AIC: 9090.
Df Residuals: 3475 BIC: 9109.
Df Model: 3
Covariance Type: nonrobust
==============================================================================
coef std err t P>|t| [0.025 0.975]
------------------------------------------------------------------------------
RELIMP -0.0836 0.016 -5.372 0.000 -0.114 -0.053
AGE -0.4253 0.015 -27.717 0.000 -0.455 -0.395
GENDER -0.0582 0.015 -3.782 0.000 -0.088 -0.028
==============================================================================
Omnibus: 12.035 Durbin-Watson: 1.977
Prob(Omnibus): 0.002 Jarque-Bera (JB): 9.991
Skew: 0.057 Prob(JB): 0.00677
Kurtosis: 2.763 Cond. No. 1.26
==============================================================================
OLS Regression Results
==============================================================================
Dep. Variable: g factor R-squared: 0.199
Model: OLS Adj. R-squared: 0.198
Method: Least Squares F-statistic: 288.0
Date: Thu, 02 Aug 2018 Prob (F-statistic): 5.32e-167
Time: 12:11:03 Log-Likelihood: -4566.8
No. Observations: 3491 AIC: 9140.
Df Residuals: 3488 BIC: 9158.
Df Model: 3
Covariance Type: nonrobust
==============================================================================
coef std err t P>|t| [0.025 0.975]
------------------------------------------------------------------------------
PRAY -0.0586 0.016 -3.718 0.000 -0.090 -0.028
AGE -0.4313 0.015 -28.260 0.000 -0.461 -0.401
GENDER -0.0600 0.016 -3.820 0.000 -0.091 -0.029
==============================================================================
Omnibus: 11.895 Durbin-Watson: 1.976
Prob(Omnibus): 0.003 Jarque-Bera (JB): 9.650
Skew: 0.043 Prob(JB): 0.00803
Kurtosis: 2.757 Cond. No. 1.33
==============================================================================
OLS Regression Results
==============================================================================
Dep. Variable: g factor R-squared: 0.201
Model: OLS Adj. R-squared: 0.201
Method: Least Squares F-statistic: 293.0
Date: Thu, 02 Aug 2018 Prob (F-statistic): 1.27e-169
Time: 12:11:03 Log-Likelihood: -4555.1
No. Observations: 3487 AIC: 9116.
Df Residuals: 3484 BIC: 9135.
Df Model: 3
Covariance Type: nonrobust
==============================================================================
coef std err t P>|t| [0.025 0.975]
------------------------------------------------------------------------------
REL -0.0780 0.015 -5.050 0.000 -0.108 -0.048
AGE -0.4275 0.015 -27.954 0.000 -0.457 -0.398
GENDER -0.0622 0.015 -4.062 0.000 -0.092 -0.032
==============================================================================
Omnibus: 11.538 Durbin-Watson: 1.967
Prob(Omnibus): 0.003 Jarque-Bera (JB): 9.534
Skew: 0.050 Prob(JB): 0.00851
Kurtosis: 2.764 Cond. No. 1.22
==============================================================================
REL: Response to "How religious are you?", on a scale of 1-4, with 1 being the least religious and 4 being the most religious RELIMP: Response to "How important is religion to you?", on a scale of 1-4, with 1 being the least important and 4 being the most important PRAY: Response to "How often do you pray?", on a scale of 1-6, with 1 being never and 6 being once or more a day
References
- ^ Lawley, D. N. (14 February 2012). "XX.—Some New Results in Maximum Likelihood Factor Analysis". Proceedings of the Royal Society of Edinburgh. Section A. Mathematical and Physical Sciences. 67 (4): 256–264. doi:10.1017/S0080454100008128.
- ^ Rubin, Donald B.; Thayer, Dorothy T. (1982). [10.1007/BF02293851 "EM algorithms for ML factor analysis"]. Psychometrika. 47 (1): 69–76. doi:10.1007/BF02293851. ISSN 0033-3123.
{{cite journal}}: Check|url=value (help) - ^ Browne, Michael; Arminger, Gerhard (1995). "Specification and Estimation of Mean- and Covariance-Structure Models". Handbook of statistical modeling for the social and behavioral sciences. p. 185-248. ISBN 978-1-4899-1292-3.
- ^ Seamans, Jeremy K.; Yang, Charles R. "The principal features and mechanisms of dopamine modulation in the prefrontal cortex". Progress in Neurobiology. pp. 1–58. doi:10.1016/j.pneurobio.2004.05.006.
- ^ Durstewitz, Daniel; Seamans, Jeremy K. (1 November 2008). "The dual-state theory of prefrontal cortex dopamine function with relevance to catechol-o-methyltransferase genotypes and schizophrenia". Biological Psychiatry. 64 (9): 739–749. doi:10.1016/j.biopsych.2008.05.015. ISSN 1873-2402.
- ^ Sklar, P. "The Genetics of Schizophrenia and Bipolar Disorder". In Charney, D; Buxmaum, J; Nestler, E (eds.). Neurobiology of Mental Illness. Oxford University Press.
- ^ McCarthy, MJ; Nievergelt, CM; Kelsoe, JR; Welsh, DK (2012). "A survey of genomic studies supports association of circadian clock genes with bipolar disorder spectrum illnesses and lithium response". PloS one. 7 (2): e32091. doi:10.1371/journal.pone.0032091. PMC 3285204. PMID 22384149.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Patel, N; Nandagopal, J; Cerullo, M; Fleck, D; Adler, C; Strakowski, S; DelBello, M. "Neuroimaging Biomarkers for Bipolar Disorder Across the Lifespan". In Ritsner, M (ed.). The Handbook of Neuropsychiatric Biomarkers, Endophenotypes and Genes: Volume II: Neuroanatomical and Neuroimaging Endophenotypes and Biomarkers. Springer.
- ^ Blond, B; Blumberg, H. "Functional Neuroimaging Research in Bipolar". In Manji, H; Zarate, C (eds.). Behavioral Neurobiology of Bipolar Disorder and its Treatment. pp. 230–240.
- ^ Charney, Dennis; Sklar, Pamela; Nestler, Eric; Buxbaum, Joseph (2013). "17". Neurobiology of Mental Illness (4 ed.). Oxford University Press. ISBN 9780199934959.
- ^ Charney et al. 2013, 18.
- ^ Sadock, Virginia; Sadock, Benjamin; Ruiz, Pedro. "12.7". Kaplan and Sadock's Comprehensive Textbook of Psychiatry (10 ed.). Wolters Kluwer Health.
- ^ Charney et al. 2013, 19.
- ^ Charney et al. 2013, 20.
- ^ Sadock, Sadock & Ruiz 2016, 12.1.
- ^ Sadock, Sadock & Ruiz 2016, 12.6.
- ^ Charney et al. 2013, chpt.23.
- ^ Hill, K; Mann, L; Laws, KR; Stephenson, CM; Nimmo-Smith, I; McKenna, PJ (October 2004). "Hypofrontality in schizophrenia: a meta-analysis of functional imaging studies". Acta psychiatrica Scandinavica. 110 (4): 243–56. doi:10.1111/j.1600-0447.2004.00376.x. PMID 15352925.
- ^ Del Casale, A; Kotzalidis, GD; Rapinesi, C; Sorice, S; Girardi, N; Ferracuti, S; Girardi, P (2016). "Functional Magnetic Resonance Imaging Correlates of First-Episode Psychoses during Attentional and Memory Task Performance". Neuropsychobiology. 74 (1): 22–31. doi:10.1159/000448620. PMID 27698323.
- ^ Bora, E; Fornito, A; Radua, J; Walterfang, M; Seal, M; Wood, SJ; Yücel, M; Velakoulis, D; Pantelis, C (April 2011). "Neuroanatomical abnormalities in schizophrenia: a multimodal voxelwise meta-analysis and meta-regression analysis". Schizophrenia research. 127 (1–3): 46–57. doi:10.1016/j.schres.2010.12.020. PMID 21300524.
- ^ Sklar, P. "The Genetics of Schizophrenia and Bipolar Disorder". In Charney, D; Buxmaum, J; Nestler, E (eds.). Neurobiology of Mental Illness. Oxford University Press.
- ^ McCarthy, MJ; Nievergelt, CM; Kelsoe, JR; Welsh, DK (2012). "A survey of genomic studies supports association of circadian clock genes with bipolar disorder spectrum illnesses and lithium response". PloS one. 7 (2): e32091. doi:10.1371/journal.pone.0032091. PMC 3285204. PMID 22384149.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Jiang, HY; Qiao, F; Xu, XF; Yang, Y; Bai, Y; Jiang, LL (9 August 2013). "Meta-analysis confirms a functional polymorphism (5-HTTLPR) in the serotonin transporter gene conferring risk of bipolar disorder in European populations". Neuroscience letters. 549: 191–6. doi:10.1016/j.neulet.2013.05.065. PMID 23756178.
- ^ Gao, J; Jia, M; Qiao, D; Qiu, H; Sokolove, J; Zhang, J; Pan, Z (March 2016). "TPH2 gene polymorphisms and bipolar disorder: A meta-analysis". American journal of medical genetics. Part B, Neuropsychiatric genetics : the official publication of the International Society of Psychiatric Genetics. 171B (2): 145–52. doi:10.1002/ajmg.b.32381. PMID 26365518.
- ^ Wang, Z; Li, Z; Gao, K; Fang, Y (24 December 2014). "Association between brain-derived neurotrophic factor genetic polymorphism Val66Met and susceptibility to bipolar disorder: a meta-analysis". BMC psychiatry. 14: 366. doi:10.1186/s12888-014-0366-9. PMC 4297385. PMID 25539739.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Patel, N; Nandagopal, J; Cerullo, M; Fleck, D; Adler, C; Strakowski, S; DelBello, M. "Neuroimaging Biomarkers for Bipolar Disorder Across the Lifespan". In Ritsner, M (ed.). The Handbook of Neuropsychiatric Biomarkers, Endophenotypes and Genes: Volume II: Neuroanatomical and Neuroimaging Endophenotypes and Biomarkers. Springer.
- ^ Blond, B; Blumberg, H. "Functional Neuroimaging Research in Bipolar". In Manji, H; Zarate, C (eds.). Behavioral Neurobiology of Bipolar Disorder and its Treatment. pp. 230–240.
- ^ Phillips, ML; Swartz, HA (August 2014). "A critical appraisal of neuroimaging studies of bipolar disorder: toward a new conceptualization of underlying neural circuitry and a road map for future research". The American journal of psychiatry. 171 (8): 829–43. doi:10.1176/appi.ajp.2014.13081008. PMC 4119497. PMID 24626773.
- ^ Nusslock, R; Young, CB; Damme, KS (November 2014). "Elevated reward-related neural activation as a unique biological marker of bipolar disorder: assessment and treatment implications". Behaviour research and therapy. 62: 74–87. doi:10.1016/j.brat.2014.08.011. PMID 25241675.
- ^ Bora, E; Fornito, A; Yücel, M; Pantelis, C (1 June 2010). "Voxelwise meta-analysis of gray matter abnormalities in bipolar disorder". Biological psychiatry. 67 (11): 1097–105. doi:10.1016/j.biopsych.2010.01.020. PMID 20303066.
- ^ Kempton, MJ; Geddes, JR; Ettinger, U; Williams, SC; Grasby, PM (September 2008). "Meta-analysis, database, and meta-regression of 98 structural imaging studies in bipolar disorder". Archives of general psychiatry. 65 (9): 1017–32. doi:10.1001/archpsyc.65.9.1017. PMID 18762588.
- ^ Arnone, D; Cavanagh, J; Gerber, D; Lawrie, SM; Ebmeier, KP; McIntosh, AM (September 2009). "Magnetic resonance imaging studies in bipolar disorder and schizophrenia: meta-analysis". The British journal of psychiatry : the journal of mental science. 195 (3): 194–201. doi:10.1192/bjp.bp.108.059717. PMID 19721106.
- ^ Selvaraj, S; Arnone, D; Job, D; Stanfield, A; Farrow, TF; Nugent, AC; Scherk, H; Gruber, O; Chen, X; Sachdev, PS; Dickstein, DP; Malhi, GS; Ha, TH; Ha, K; Phillips, ML; McIntosh, AM (March 2012). "Grey matter differences in bipolar disorder: a meta-analysis of voxel-based morphometry studies". Bipolar disorders. 14 (2): 135–45. doi:10.1111/j.1399-5618.2012.01000.x. PMID 22420589.
- ^ Heckers, Stephan; Woodward, Neil; Öngür, Dost (2018). "Neuroimaging of Psychotic Disorders". In Sklar, Pamela; Charney, Dennis; Buxbaum, Joseph; Nestler, Eric (eds.). Neurobiology of Mental Illness (5th edition ed.). Oxford University Press. ISBN 9780190681425.
{{cite book}}:|edition=has extra text (help) - ^ Hajek, T; Alda, M; Hajek, E; Ivanoff, J (December 2013). "Functional neuroanatomy of response inhibition in bipolar disorders--combined voxel based and cognitive performance meta-analysis". Journal of psychiatric research. 47 (12): 1955–66. doi:10.1016/j.jpsychires.2013.08.015. PMID 24070910.
- ^ Chen, CH; Suckling, J; Lennox, BR; Ooi, C; Bullmore, ET (February 2011). "A quantitative meta-analysis of fMRI studies in bipolar disorder". Bipolar disorders. 13 (1): 1–15. doi:10.1111/j.1399-5618.2011.00893.x. PMID 21320248.
- ^ Gigante, AD; Bond, DJ; Lafer, B; Lam, RW; Young, LT; Yatham, LN (August 2012). "Brain glutamate levels measured by magnetic resonance spectroscopy in patients with bipolar disorder: a meta-analysis". Bipolar disorders. 14 (5): 478–87. doi:10.1111/j.1399-5618.2012.01033.x. PMID 22834460.
- ^ Chitty, KM; Lagopoulos, J; Lee, RS; Hickie, IB; Hermens, DF (November 2013). "A systematic review and meta-analysis of proton magnetic resonance spectroscopy and mismatch negativity in bipolar disorder". European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology. 23 (11): 1348–63. doi:10.1016/j.euroneuro.2013.07.007. PMID 23968965.
- ^ Kraguljac, NV; Reid, M; White, D; Jones, R; den Hollander, J; Lowman, D; Lahti, AC (NaN). "Neurometabolites in schizophrenia and bipolar disorder - a systematic review and meta-analysis". Psychiatry research. 203 (2–3): 111–25. doi:10.1016/j.pscychresns.2012.02.003. PMC 3466386. PMID 22981426.
{{cite journal}}: Check date values in:|date=(help) - ^ Manji & Zarate 2011, p. 107.
- ^ van Enkhuizen, J; Janowsky, DS; Olivier, B; Minassian, A; Perry, W; Young, JW; Geyer, MA (15 April 2015). "The catecholaminergic-cholinergic balance hypothesis of bipolar disorder revisited". European journal of pharmacology. 753: 114–26. doi:10.1016/j.ejphar.2014.05.063. PMC 4318788. PMID 25107282.
- ^ a b Manji, HK; Quiroz, JA; Payne, JL; Singh, J; Lopes, BP; Viegas, JS; Zarate, CA (October 2003). "The underlying neurobiology of bipolar disorder". World psychiatry : official journal of the World Psychiatric Association (WPA). 2 (3): 136–46. PMC 1525098. PMID 16946919.
- ^ Manji & Zarate 2011, p. 110.
- ^ Manji & Zarate 2011, p. 112.
- ^ Belvederi Murri, M; Prestia, D; Mondelli, V; Pariante, C; Patti, S; Olivieri, B; Arzani, C; Masotti, M; Respino, M; Antonioli, M; Vassallo, L; Serafini, G; Perna, G; Pompili, M; Amore, M (January 2016). "The HPA axis in bipolar disorder: Systematic review and meta-analysis". Psychoneuroendocrinology. 63: 327–42. doi:10.1016/j.psyneuen.2015.10.014. PMID 26547798.
- ^ Manji & Zarate 2011, p. 142-145.
- ^ Manji & Zarate 2011, p. 151.
- ^ Manji & Zarate 2011, p. 193.
- ^ Manji & Zarate 2011, p. 125-130.
- ^ Manji & Zarate 2011, p. 143.
- ^ Muneer, A (January 2016). "The Neurobiology of Bipolar Disorder: An Integrated Approach". Chonnam medical journal. 52 (1): 18–37. doi:10.4068/cmj.2016.52.1.18. PMC 4742607. PMID 26865997.
- ^ Insel, TR (11 November 2010). "Rethinking schizophrenia". Nature. 468 (7321): 187–93. doi:10.1038/nature09552. PMID 21068826.
- ^ Kahn, RS; Sommer, IE (February 2015). "The neurobiology and treatment of first-episode schizophrenia". Molecular psychiatry. 20 (1): 84–97. doi:10.1038/mp.2014.66. PMC 4320288. PMID 25048005.
- ^ Fusar-Poli, P; Meyer-Lindenberg, A (January 2013). "Striatal presynaptic dopamine in schizophrenia, part II: meta-analysis of [(18)F/(11)C]-DOPA PET studies". Schizophrenia bulletin. 39 (1): 33–42. doi:10.1093/schbul/sbr180. PMC 3523905. PMID 22282454.
- ^ Howes, OD; Kambeitz, J; Kim, E; Stahl, D; Slifstein, M; Abi-Dargham, A; Kapur, S (August 2012). "The nature of dopamine dysfunction in schizophrenia and what this means for treatment". Archives of general psychiatry. 69 (8): 776–86. doi:10.1001/archgenpsychiatry.2012.169. PMC 3730746. PMID 22474070.
- ^ a b Broyd, A; Balzan, RP; Woodward, TS; Allen, P (June 2017). "Dopamine, cognitive biases and assessment of certainty: A neurocognitive model of delusions". Clinical psychology review. 54: 96–106. doi:10.1016/j.cpr.2017.04.006. PMID 28448827.
- ^ Howes, OD; Murray, RM (10 May 2014). "Schizophrenia: an integrated sociodevelopmental-cognitive model". Lancet (London, England). 383 (9929): 1677–1687. doi:10.1016/S0140-6736(13)62036-X. PMC 4127444. PMID 24315522.
- ^ Grace, AA (August 2016). "Dysregulation of the dopamine system in the pathophysiology of schizophrenia and depression". Nature reviews. Neuroscience. 17 (8): 524–32. doi:10.1038/nrn.2016.57. PMC 5166560. PMID 27256556.
- ^ a b Corlett, PR; Taylor, JR; Wang, XJ; Fletcher, PC; Krystal, JH (November 2010). "Toward a neurobiology of delusions". Progress in neurobiology. 92 (3): 345–69. doi:10.1016/j.pneurobio.2010.06.007. PMC 3676875. PMID 20558235.
- ^ Heckers, S; Konradi, C (September 2015). "GABAergic mechanisms of hippocampal hyperactivity in schizophrenia". Schizophrenia research. 167 (1–3): 4–11. doi:10.1016/j.schres.2014.09.041. PMC 4402105. PMID 25449711.
- ^ Goldman-Rakic, PS; Castner, SA; Svensson, TH; Siever, LJ; Williams, GV (June 2004). "Targeting the dopamine D1 receptor in schizophrenia: insights for cognitive dysfunction". Psychopharmacology. 174 (1): 3–16. doi:10.1007/s00213-004-1793-y. PMID 15118803.
- ^ Arnsten, AF; Girgis, RR; Gray, DL; Mailman, RB (1 January 2017). "Novel Dopamine Therapeutics for Cognitive Deficits in Schizophrenia". Biological psychiatry. 81 (1): 67–77. doi:10.1016/j.biopsych.2015.12.028. PMC 4949134. PMID 26946382.
- ^ Abi-Dargham, A; Moore, H (October 2003). "Prefrontal DA transmission at D1 receptors and the pathology of schizophrenia". The Neuroscientist : a review journal bringing neurobiology, neurology and psychiatry. 9 (5): 404–16. doi:10.1177/1073858403252674. PMID 14580124.
- ^ Maia, TV; Frank, MJ (1 January 2017). "An Integrative Perspective on the Role of Dopamine in Schizophrenia". Biological psychiatry. 81 (1): 52–66. doi:10.1016/j.biopsych.2016.05.021. PMC 5486232. PMID 27452791.
- ^ Kambeitz, J; Abi-Dargham, A; Kapur, S; Howes, OD (June 2014). "Alterations in cortical and extrastriatal subcortical dopamine function in schizophrenia: systematic review and meta-analysis of imaging studies". The British journal of psychiatry : the journal of mental science. 204 (6): 420–9. doi:10.1192/bjp.bp.113.132308. PMID 25029687.
- ^ Catts, VS; Lai, YL; Weickert, CS; Weickert, TW; Catts, SV (April 2016). "A quantitative review of the postmortem evidence for decreased cortical N-methyl-D-aspartate receptor expression levels in schizophrenia: How can we link molecular abnormalities to mismatch negativity deficits?". Biological psychology. 116: 57–67. doi:10.1016/j.biopsycho.2015.10.013. PMID 26549579.
- ^ Michie, PT; Malmierca, MS; Harms, L; Todd, J (April 2016). "The neurobiology of MMN and implications for schizophrenia". Biological psychology. 116: 90–7. doi:10.1016/j.biopsycho.2016.01.011. PMID 26826620.
- ^ Pratt, J; Dawson, N; Morris, BJ; Grent-'t-Jong, T; Roux, F; Uhlhaas, PJ (February 2017). "Thalamo-cortical communication, glutamatergic neurotransmission and neural oscillations: A unique window into the origins of ScZ?". Schizophrenia research. 180: 4–12. doi:10.1016/j.schres.2016.05.013. PMID 27317361.
- ^ Merritt, K; Egerton, A; Kempton, MJ; Taylor, MJ; McGuire, PK (1 July 2016). "Nature of Glutamate Alterations in Schizophrenia: A Meta-analysis of Proton Magnetic Resonance Spectroscopy Studies". JAMA psychiatry. 73 (7): 665–74. doi:10.1001/jamapsychiatry.2016.0442. PMID 27304221.
We found significant differences in glutamatergicmetabo- lites across several cortical and subcortical regions in cases compared with controls. Although the nature of the findings varied depending on the patient subgroup and brain region, all of the significant findings reflected elevations in glutama- tergic metabolites in patients and HR individuals. This find- ing is consistent with data from animal models of schizo- phrenia that propose an increase in glutamatergic activity resulting from NMDAR hypofunction.66 The finding is also consistent with human studies of NMDAR hypofunction that show increases in both glutamate and glutamine concentra- tions in the cortex following ketamine administration to healthy volunteers.
- ^ Marsman, A; van den Heuvel, MP; Klomp, DW; Kahn, RS; Luijten, PR; Hulshoff Pol, HE (January 2013). "Glutamate in schizophrenia: a focused review and meta-analysis of ¹H-MRS studies". Schizophrenia bulletin. 39 (1): 120–9. doi:10.1093/schbul/sbr069. PMC 3523901. PMID 21746807.
- ^ Cohen, SM; Tsien, RW; Goff, DC; Halassa, MM (September 2015). "The impact of NMDA receptor hypofunction on GABAergic neurons in the pathophysiology of schizophrenia". Schizophrenia research. 167 (1–3): 98–107. doi:10.1016/j.schres.2014.12.026. PMC 4724170. PMID 25583246.
- ^ Marín, O (18 January 2012). "Interneuron dysfunction in psychiatric disorders". Nature reviews. Neuroscience. 13 (2): 107–20. doi:10.1038/nrn3155. PMID 22251963.
- ^ Taylor, SF; Tso, IF (September 2015). "GABA abnormalities in schizophrenia: a methodological review of in vivo studies". Schizophrenia research. 167 (1–3): 84–90. doi:10.1016/j.schres.2014.10.011. PMC 4409914. PMID 25458856.
- ^ Egerton, A; Modinos, G; Ferrera, D; McGuire, P (6 June 2017). "Neuroimaging studies of GABA in schizophrenia: a systematic review with meta-analysis". Translational psychiatry. 7 (6): e1147. doi:10.1038/tp.2017.124. PMC 5537645. PMID 28585933.
- ^ Marín, O (18 January 2012). "Interneuron dysfunction in psychiatric disorders". Nature reviews. Neuroscience. 13 (2): 107–20. doi:10.1038/nrn3155. PMID 22251963.
- ^ Lewis, DA; Hashimoto, T; Volk, DW (April 2005). "Cortical inhibitory neurons and schizophrenia". Nature reviews. Neuroscience. 6 (4): 312–24. doi:10.1038/nrn1648. PMID 15803162.
- ^ Senkowski, D; Gallinat, J (15 June 2015). "Dysfunctional prefrontal gamma-band oscillations reflect working memory and other cognitive deficits in schizophrenia". Biological psychiatry. 77 (12): 1010–9. doi:10.1016/j.biopsych.2015.02.034. PMID 25847179.
- ^ Tse, MT; Piantadosi, PT; Floresco, SB (1 June 2015). "Prefrontal cortical gamma-aminobutyric acid transmission and cognitive function: drawing links to schizophrenia from preclinical research". Biological psychiatry. 77 (11): 929–39. doi:10.1016/j.biopsych.2014.09.007. PMID 25442792.
- ^ Gonzalez-Burgos, G; Cho, RY; Lewis, DA (15 June 2015). "Alterations in cortical network oscillations and parvalbumin neurons in schizophrenia". Biological psychiatry. 77 (12): 1031–40. doi:10.1016/j.biopsych.2015.03.010. PMC 4444373. PMID 25863358.
- ^ Piper, M; Beneyto, M; Burne, TH; Eyles, DW; Lewis, DA; McGrath, JJ (September 2012). "The neurodevelopmental hypothesis of schizophrenia: convergent clues from epidemiology and neuropathology". The Psychiatric clinics of North America. 35 (3): 571–84. doi:10.1016/j.psc.2012.06.002. PMID 22929867.
- ^ Birnbaum, R; Weinberger, DR (December 2017). "Genetic insights into the neurodevelopmental origins of schizophrenia". Nature reviews. Neuroscience. 18 (12): 727–740. doi:10.1038/nrn.2017.125. PMID 29070826.
- ^ Khandaker, GM; Zimbron, J; Lewis, G; Jones, PB (February 2013). "Prenatal maternal infection, neurodevelopment and adult schizophrenia: a systematic review of population-based studies". Psychological medicine. 43 (2): 239–57. doi:10.1017/S0033291712000736. PMC 3479084. PMID 22717193.
- ^ Brown, AS; Derkits, EJ (March 2010). "Prenatal infection and schizophrenia: a review of epidemiologic and translational studies". The American journal of psychiatry. 167 (3): 261–80. doi:10.1176/appi.ajp.2009.09030361. PMC 3652286. PMID 20123911.
- ^ Brown, AS (January 2011). "The environment and susceptibility to schizophrenia". Progress in neurobiology. 93 (1): 23–58. doi:10.1016/j.pneurobio.2010.09.003. PMC 3521525. PMID 20955757.
- ^ Negrón-Oyarzo, I; Lara-Vásquez, A; Palacios-García, I; Fuentealba, P; Aboitiz, F (11 March 2016). "Schizophrenia and reelin: a model based on prenatal stress to study epigenetics, brain development and behavior". Biological research. 49: 16. doi:10.1186/s40659-016-0076-5. PMC 4787713. PMID 26968981.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Cannon, TD (December 2015). "How Schizophrenia Develops: Cognitive and Brain Mechanisms Underlying Onset of Psychosis". Trends in cognitive sciences. 19 (12): 744–756. doi:10.1016/j.tics.2015.09.009. PMC 4673025. PMID 26493362.
- ^ Lesh, TA; Niendam, TA; Minzenberg, MJ; Carter, CS (January 2011). "Cognitive control deficits in schizophrenia: mechanisms and meaning". Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 36 (1): 316–38. doi:10.1038/npp.2010.156. PMC 3052853. PMID 20844478.
- ^ Barch, DM; Ceaser, A (January 2012). "Cognition in schizophrenia: core psychological and neural mechanisms". Trends in cognitive sciences. 16 (1): 27–34. doi:10.1016/j.tics.2011.11.015. PMC 3860986. PMID 22169777.
- ^ a b Eisenberg, DP; Berman, KF (January 2010). "Executive function, neural circuitry, and genetic mechanisms in schizophrenia". Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 35 (1): 258–77. doi:10.1038/npp.2009.111. PMC 2794926. PMID 19693005.
- ^ Osimo, EF; Beck, K; Reis Marques, T; Howes, OD (6 March 2018). "Synaptic loss in schizophrenia: a meta-analysis and systematic review of synaptic protein and mRNA measures". Molecular psychiatry. doi:10.1038/s41380-018-0041-5. PMC 6004314. PMID 29511299.
- ^ Walton, E; Hibar, DP; van Erp, TG; Potkin, SG; Roiz-Santiañez, R; Crespo-Facorro, B; Suarez-Pinilla, P; Van Haren, NE; de Zwarte, SM; Kahn, RS; Cahn, W; Doan, NT; Jørgensen, KN; Gurholt, TP; Agartz, I; Andreassen, OA; Westlye, LT; Melle, I; Berg, AO; Mørch-Johnsen, L; Faerden, A; Flyckt, L; Fatouros-Bergman, H; Karolinska Schizophrenia Project Consortium, (KaSP).; Jönsson, EG; Hashimoto, R; Yamamori, H; Fukunaga, M; Preda, A; De Rossi, P; Piras, F; Banaj, N; Ciullo, V; Spalletta, G; Gur, RE; Gur, RC; Wolf, DH; Satterthwaite, TD; Beard, LM; Sommer, IE; Koops, S; Gruber, O; Richter, A; Krämer, B; Kelly, S; Donohoe, G; McDonald, C; Cannon, DM; Corvin, A; Gill, M; Di Giorgio, A; Bertolino, A; Lawrie, S; Nickson, T; Whalley, HC; Neilson, E; Calhoun, VD; Thompson, PM; Turner, JA; Ehrlich, S (May 2017). "Positive symptoms associate with cortical thinning in the superior temporal gyrus via the ENIGMA Schizophrenia consortium". Acta psychiatrica Scandinavica. 135 (5): 439–447. doi:10.1111/acps.12718. PMC 5399182. PMID 28369804.
- ^ Walton, E; Hibar, DP; van Erp, TGM; Potkin, SG; Roiz-Santiañez, R; Crespo-Facorro, B; Suarez-Pinilla, P; van Haren, NEM; de Zwarte, SMC; Kahn, RS; Cahn, W; Doan, NT; Jørgensen, KN; Gurholt, TP; Agartz, I; Andreassen, OA; Westlye, LT; Melle, I; Berg, AO; Morch-Johnsen, L; Færden, A; Flyckt, L; Fatouros-Bergman, H; Karolinska Schizophrenia Project Consortium, (KaSP).; Jönsson, EG; Hashimoto, R; Yamamori, H; Fukunaga, M; Jahanshad, N; De Rossi, P; Piras, F; Banaj, N; Spalletta, G; Gur, RE; Gur, RC; Wolf, DH; Satterthwaite, TD; Beard, LM; Sommer, IE; Koops, S; Gruber, O; Richter, A; Krämer, B; Kelly, S; Donohoe, G; McDonald, C; Cannon, DM; Corvin, A; Gill, M; Di Giorgio, A; Bertolino, A; Lawrie, S; Nickson, T; Whalley, HC; Neilson, E; Calhoun, VD; Thompson, PM; Turner, JA; Ehrlich, S (January 2018). "Prefrontal cortical thinning links to negative symptoms in schizophrenia via the ENIGMA consortium". Psychological medicine. 48 (1): 82–94. doi:10.1017/S0033291717001283. PMC 5826665. PMID 28545597.
- ^ Javitt, DC; Sweet, RA (September 2015). "Auditory dysfunction in schizophrenia: integrating clinical and basic features". Nature reviews. Neuroscience. 16 (9): 535–50. doi:10.1038/nrn4002. PMC 4692466. PMID 26289573.
- ^ Cohen, AS; Minor, KS (January 2010). "Emotional experience in patients with schizophrenia revisited: meta-analysis of laboratory studies". Schizophrenia bulletin. 36 (1): 143–50. doi:10.1093/schbul/sbn061. PMC 2800132. PMID 18562345.
- ^ Strauss, GP; Gold, JM (April 2012). "A new perspective on anhedonia in schizophrenia". The American journal of psychiatry. 169 (4): 364–73. doi:10.1176/appi.ajp.2011.11030447. PMC 3732829. PMID 22407079.
- ^ Young, Jared; Anticevic, Alan; Barch, Deanna (2018). "Cognitive and Motivational Neuroscience of Psychotic Disorders". In Charney, Dennis; Buxbaum, Joseph; Sklar, Pamela; Nestler, Eric (eds.). Charney & Nestler's Neurobiology of Mental Illness (5th ed.). New York: Oxford University Press. pp. 215, 217. ISBN 9780190681425.
Several recent reviews (e.g., Cohen and Minor, 2010) have found that individuals with schizophrenia show relatively intact self-reported emotional responses to affect-eliciting stimuli as well as other indicators of intact response(215)...Taken together, the literature increasingly suggests that there may be a deficit in putatively DA-mediated reward learning and/ or reward prediction functions in schizophrenia. Such findings suggest that impairment in striatal reward prediction mechanisms may influence "wanting" in schizophrenia in a way that reduces the ability of individuals with schizophrenia to use anticipated rewards to drive motivated behavior.(217)
- ^ Chase, HW; Loriemi, P; Wensing, T; Eickhoff, SB; Nickl-Jockschat, T (July 2018). "Meta-analytic evidence for altered mesolimbic responses to reward in schizophrenia". Human brain mapping. 39 (7): 2917–2928. doi:10.1002/hbm.24049. PMID 29573046.
Specifically, a reduced anticipatory response might result from a reduction in the learning rate, and reflect a slower transfer from outcome to reward-related responses. This account would predict intact or enhanced outcome-locked activation, with reduced anticipatory activation. This account is also consistent with behavioral evidence of reinforcement learning deficits in SCZ (Waltz et al., 2007) and outcome-locked null results (Culbreth, West- brook, Xu, Barch, & Waltz, 2016b).
- ^ Fletcher, PC; Frith, CD (January 2009). "Perceiving is believing: a Bayesian approach to explaining the positive symptoms of schizophrenia". Nature reviews. Neuroscience. 10 (1): 48–58. doi:10.1038/nrn2536. PMID 19050712.
- ^ Friston, KJ; Stephan, KE; Montague, R; Dolan, RJ (July 2014). "Computational psychiatry: the brain as a phantastic organ". The lancet. Psychiatry. 1 (2): 148–58. doi:10.1016/S2215-0366(14)70275-5. PMID 26360579.
- ^ Sterzer, Philipp; Adams, Rick A.; Fletcher, Paul; Frith, Chris; Lawrie, Stephen M.; Muckli, Lars; Petrovic, Predrag; Uhlhaas, Peter; Voss, Martin; Corlett, Philip R. (May 2018). "The Predictive Coding Account of Psychosis". Biological Psychiatry. doi:10.1016/j.biopsych.2018.05.015.
- ^ Friston, K; Brown, HR; Siemerkus, J; Stephan, KE (October 2016). "The dysconnection hypothesis (2016)". Schizophrenia research. 176 (2–3): 83–94. doi:10.1016/j.schres.2016.07.014. PMC 5147460. PMID 27450778.
- ^ Fletcher, PC; Frith, CD (January 2009). "Perceiving is believing: a Bayesian approach to explaining the positive symptoms of schizophrenia". Nature reviews. Neuroscience. 10 (1): 48–58. doi:10.1038/nrn2536. PMID 19050712.
- ^ Corlett, PR; Honey, GD; Krystal, JH; Fletcher, PC (January 2011). "Glutamatergic model psychoses: prediction error, learning, and inference". Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 36 (1): 294–315. doi:10.1038/npp.2010.163. PMC 3055519. PMID 20861831.






































![{\displaystyle x=z\Lambda +\epsilon ;\quad E[zz']=\Phi ;\quad E[\epsilon \epsilon ']=\Psi ={\text{diag}}(\psi _{1},\psi _{2}\dots \psi _{p});\quad E[xx']=\Lambda \Phi \Lambda '+\Psi }](https://wikimedia.org/api/rest_v1/media/math/render/svg/a82c9a2d65f3061476531ac477e70ff4a9ddb389)





![{\displaystyle E[X^{2}X^{2}]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/250991bf9d424b24e51e65584df3dc73dd6b9ddc)



![{\displaystyle \theta =\left[{\text{vec}}(\Lambda ),{\text{vech}}(\Psi ),{\text{vech}}(\Psi )\right]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/f177c94680ab54b4818c3ec6bdeaab21197ae55a)



![{\displaystyle {\mathcal {I}}_{exp}=\left[\Delta '(\Sigma ^{-1}\otimes \Sigma ^{-1})\Delta \right]^{-1}}](https://wikimedia.org/api/rest_v1/media/math/render/svg/72cd961a6e8d75affefbab8d13bd537ce9f13eec)