CD135
| FLT3 | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | FLT3, CD135, FLK-2, FLK2, STK1, fms related tyrosine kinase 3, fms related receptor tyrosine kinase 3 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | OMIM: 136351; MGI: 95559; HomoloGene: 3040; GeneCards: FLT3; OMA:FLT3 - orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Cluster of differentiation antigen 135 (CD135) also known as fms like tyrosine kinase 3 (FLT-3 with fms standing for "feline McDonough sarcoma"), receptor-type tyrosine-protein kinase FLT3, or fetal liver kinase-2 (Flk2) is a protein that in humans is encoded by the FLT3 gene. FLT3 is a cytokine receptor which belongs to the receptor tyrosine kinase class III. CD135 is the receptor for the cytokine Flt3 ligand (FLT3L).
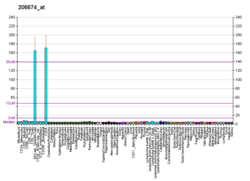
It is expressed on the surface of many hematopoietic progenitor cells. Signalling of FLT3 is important for the normal development of haematopoietic stem cells and progenitor cells.
The FLT3 gene is one of the most frequently mutated genes in acute myeloid leukemia (AML).[5] High levels of wild-type FLT3 have been reported for blast cells of some AML patients without FLT3 mutations. These high levels may be associated with worse prognosis.
Structure
FLT3 is composed of five extracellular immunoglobulin-like domains, an extracellular domain, a transmembrane domain, a juxtamembrane domain and a tyrosine-kinase domain consisting of 2 lobes that are connected by a tyrosine-kinase insert. Cytoplasmic FLT3 undergoes glycosylation, which promotes localization of the receptor to the membrane.[6]
Function
CD135 is a class III receptor tyrosine kinase. When this receptor binds to FLT3L a ternary complex is formed in which two FLT3 molecules are bridged by one (homodimeric) FLT3L.[7] The formation of such complex brings the two intracellular domains in close proximity to each other, eliciting initial trans-phosphorylation of each kinase domain. This initial phosphorylation event further activates the intrinsic tyrosine kinase activity, which in turn phosphorylates and activates signal transduction molecules that propagate the signal in the cell. Signaling through CD135 plays a role in cell survival, proliferation, and differentiation. CD135 is important for lymphocyte (B cell and T cell) development.
Two cytokines that down modulate FLT3 activity (& block FLT3-induced hematopoietic activity) are:
- TNF-alpha (Tumor necrosis factor-alpha)
- TGF-beta (Transforming growth factor-beta)
TGF-beta especially, decreases FLT3 protein levels and reverses the FLT3L-induced decrease in the time that hematopoietic progenitors spend in the G1-phase of the cell cycle.[6]
Clinical significance
Cell surface marker
Cluster of differentiation (CD) molecules are markers on the cell surface, as recognized by specific sets of antibodies, used to identify the cell type, stage of differentiation and activity of a cell. In mice, CD135 is expressed on several hematopoietic (blood) cells, including long- and short-term reconstituting hematopoietic stem cells (HSC) and other progenitors like multipotent progenitors (MPPs) and common lymphoid progenitors (CLP).[8]
Role in cancer
CD135 is a proto-oncogene, meaning that mutations of this protein can lead to cancer.[9] Mutations of the FLT3 receptor can lead to the development of leukemia, a cancer of bone marrow hematopoietic progenitors. Internal tandem duplications of FLT3 (FLT3-ITD) are the most common mutations associated with acute myelogenous leukemia (AML) and are a prognostic indicator associated with adverse disease outcome.
FLT3 inhibitors
Gilteritinib, a dual FLT3-AXL tyrosine kinase inhibitor[10] has completed a phase 3 trial of relapsed/refractory acute myeloid leukemia in patients with FLT3 ITD or TKD mutations.[11] In 2017, gilteritinib gained FDA orphan drug status for AML.[12] In November 2018, the FDA approved gilteritinib (Xospata) for treatment of adult patients with relapsed or refractory acute myeloid leukemia (AML) with a FLT3 mutation as detected by an FDA-approved test.[13]
In July 2023, quizartinib (Vanflyta) was also approved for the treatment of newly diagnosed AML with FLT3 internal tandem duplication (ITD)-positive, as detected by an FDA-approved test.[14] Precisely, it should be used with standard cytarabine and anthracycline induction and cytarabine consolidation, and as maintenance monotherapy following consolidation chemotherapy.[14]
Midostaurin was approved by the FDA in April 2017 for the treatment of adult patients with newly diagnosed AML who are positive for oncogenic FLT3, in combination with chemotherapy.[15] The drug is approved for use with a companion diagnostic, the LeukoStrat CDx FLT3 Mutation Assay, which is used to detect the FLT3 mutation in patients with AML.
Sorafenib has been reported to show significant activity against Flt3-ITD positive acute myelogenous leukemia.[16][17]
Sunitinib also inhibits Flt3.
Lestaurtinib is in clinical trials.
A paper published in Nature in April 2012 studied patients who developed resistance to FLT3 inhibitors, finding specific DNA sites contributing to that resistance and highlighting opportunities for future development of inhibitors that could take into account the resistance-conferring mutations for a more potent treatment.[18]
See also
References
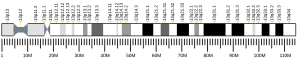
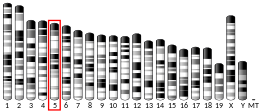
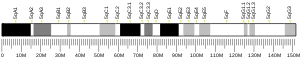
- ^ a b c GRCh38: Ensembl release 89: ENSG00000122025 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000042817 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Yamamoto Y, Kiyoi H, Nakano Y, Suzuki R, Kodera Y, Miyawaki S, Asou N, Kuriyama K, Yagasaki F, Shimazaki C, Akiyama H, Saito K, Nishimura M, Motoji T, Shinagawa K, Takeshita A, Saito H, Ueda R, Ohno R, Naoe T (April 2001). "Activating mutation of D835 within the activation loop of FLT3 in human hematologic malignancies". Blood. 97 (8): 2434–9. doi:10.1182/blood.V97.8.2434. PMID 11290608.
- ^ a b "FLT3 Signaling". Pathway Central. SABiosciences. Archived from the original on 2017-11-11. Retrieved 2012-12-18.
- ^ Verstraete K, Vandriessche G, Januar M, Elegheert J, Shkumatov AV, Desfosses A, Van Craenenbroeck K, Svergun DI, Gutsche I, Vergauwen B, Savvides SN (February 2011). "Structural insights into the extracellular assembly of the hematopoietic Flt3 signaling complex". Blood. 118 (1): 60–68. doi:10.1182/blood-2011-01-329532. PMID 21389326.
- ^ Mooney CJ, Cunningham A, Tsapogas P, Toellner KM, Brown G (May 2017). "Selective Expression of Flt3 within the Mouse Hematopoietic Stem Cell Compartment". Int J Mol Sci. 18 (5). doi:10.3390/ijms18051037. PMC 5454949. PMID 28498310.
- ^ Huret J-L. "FLT3 (FMS-like tyrosine kinase 3)". Atlas of Genetics and Cytogenetics in Oncology and Haematology. University Hospital of Poitiers.
- ^ Chew S, Mackey MC, Jabbour E (2020). "Gilteritinib in the treatment of relapsed and refractory acute myeloid leukemia with a FLT3 mutation". Review. Therapeutic Advances in Hematology. 11: 2040620720930614. doi:10.1177/2040620720930614. PMC 7271272. PMID 32547718.
- ^ Perl AE, Martinelli G, Cortes JE, Neubauer A, Berman E, Paolini S, et al. (October 2019). "FLT3-Mutated AML". The New England Journal of Medicine. 381 (18): 1728–1740. doi:10.1056/NEJMoa1902688. PMID 31665578.
- ^ "Gilteritinib Granted Orphan Drug Status for Acute Myeloid Leukemia". 20 July 2017.
- ^ "FDA approves gilteritinib for relapsed or refractory acute myeloid leukemia (AML) with a FLT3 mutatation". Drugs. FDA. December 14, 2018. Retrieved July 21, 2023.
- ^ a b "FDA approves quizartinib for newly diagnosed acute myeloid leukemia". Drugs. FDA. July 20, 2023. Retrieved July 21, 2023.
- ^ Office of the Commissioner. "Press Announcements - FDA approves new combination treatment for acute myeloid leukemia". www.fda.gov. Retrieved 2017-05-04.
- ^ Metzelder S, Wang Y, Wollmer E, Wanzel M, Teichler S, Chaturvedi A, Eilers M, Enghofer E, Neubauer A, Burchert A (June 2009). "Compassionate use of sorafenib in FLT3-ITD-positive acute myeloid leukemia: sustained regression before and after allogeneic stem cell transplantation". Blood. 113 (26): 6567–71. doi:10.1182/blood-2009-03-208298. PMID 19389879. S2CID 206878993.
- ^ Zhang W, Konopleva M, Shi YX, McQueen T, Harris D, Ling X, Estrov Z, Quintás-Cardama A, Small D, Cortes J, Andreeff M (February 2008). "Mutant FLT3: a direct target of sorafenib in acute myelogenous leukemia". J. Natl. Cancer Inst. 100 (3): 184–98. doi:10.1093/jnci/djm328. PMID 18230792.
- ^ Smith CC, Wang Q, Chin CS, Salerno S, Damon LE, Levis MJ, et al. (April 2012). "Validation of ITD mutations in FLT3 as a therapeutic target in human acute myeloid leukaemia". Nature. 485 (7397): 260–3. Bibcode:2012Natur.485..260S. doi:10.1038/nature11016. PMC 3390926. PMID 22504184.
Further reading
- Kazi JU, Rönnstrand L (2019). "FMS-like Tyrosine Kinase 3/FLT3: From Basic Science to Clinical Implications". Physiol Rev. 99 (3): 1433–1466. doi:10.1152/physrev.00029.2018. PMID 31066629.
- Reilly JT (2003). "FLT3 and its role in the pathogenesis of acute myeloid leukaemia". Leuk. Lymphoma. 44 (1): 1–7. doi:10.1080/1042819021000040233. PMID 12691136. S2CID 28533250.
- Kottaridis PD, Gale RE, Linch DC (2003). "Prognostic implications of the presence of FLT3 mutations in patients with acute myeloid leukemia". Leuk. Lymphoma. 44 (6): 905–13. doi:10.1080/1042819031000067503. PMID 12854887. S2CID 44447515.
- Gilliland DG (2004). "FLT3-activating mutations in acute promyelocytic leukaemia: a rationale for risk-adapted therapy with FLT3 inhibitors". Best Practice & Research. Clinical Haematology. 16 (3): 409–17. doi:10.1016/S1521-6926(03)00063-X. PMID 12935959.
- Drexler HG, Quentmeier H (2005). "FLT3: receptor and ligand". Growth Factors. 22 (2): 71–3. doi:10.1080/08977190410001700989. PMID 15253381. S2CID 86614476.
- Naoe T, Kiyoi H (2005). "Normal and oncogenic FLT3". Cell. Mol. Life Sci. 61 (23): 2932–8. doi:10.1007/s00018-004-4274-x. PMID 15583855. S2CID 27189321.
- Sternberg DW, Licht JD (2005). "Therapeutic intervention in leukemias that express the activated fms-like tyrosine kinase 3 (FLT3): opportunities and challenges". Curr. Opin. Hematol. 12 (1): 7–13. doi:10.1097/01.moh.0000147891.06584.d7. PMID 15604885. S2CID 1590938.
- Marcucci G, Mrózek K, Bloomfield CD (2005). "Molecular heterogeneity and prognostic biomarkers in adults with acute myeloid leukemia and normal cytogenetics". Curr. Opin. Hematol. 12 (1): 68–75. doi:10.1097/01.moh.0000149608.29685.d1. PMID 15604894. S2CID 6183391.
- Markovic A, MacKenzie KL, Lock RB (2005). "FLT-3: a new focus in the understanding of acute leukemia". Int. J. Biochem. Cell Biol. 37 (6): 1168–72. doi:10.1016/j.biocel.2004.12.005. PMID 15778081.
- Zheng R, Small D (2006). "Mutant FLT3 signaling contributes to a block in myeloid differentiation". Leuk. Lymphoma. 46 (12): 1679–87. doi:10.1080/10428190500261740. PMID 16263569. S2CID 20518363.
- Parcells BW, Ikeda AK, Simms-Waldrip T, et al. (2007). "FMS-like tyrosine kinase 3 in normal hematopoiesis and acute myeloid leukemia". Stem Cells. 24 (5): 1174–84. doi:10.1634/stemcells.2005-0519. PMID 16410383.
- Stubbs MC, Armstrong SA (2007). "FLT3 as a therapeutic target in childhood acute leukemia". Current Drug Targets. 8 (6): 703–14. doi:10.2174/138945007780830782. PMID 17584026.
External links
- CD135+Antigen at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Human FLT3 genome location and FLT3 gene details page in the UCSC Genome Browser.
- Overview of all the structural information available in the PDB for UniProt: P36888 (Receptor-type tyrosine-protein kinase FLT3) at the PDBe-KB.