Amphiregulin
| AREG | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | AREG, AR, AREGB, CRDGF, SDGF, amphiregulin | ||||||||||||||||||||||||||||||||||||||||||||||||||
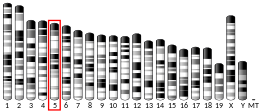
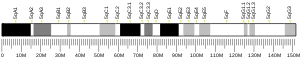
| External IDs | OMIM: 104640; MGI: 88068; HomoloGene: 1252; GeneCards: AREG; OMA:AREG - orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Amphiregulin, also known as AREG, is a protein synthesized as a transmembrane glycoprotein with 252 aminoacids and it is encoded by the AREG gene.[5][6][7] in humans.[8]
Function
The protein encoded by this gene is a member of the epidermal growth factor (EGF) family.[5]
It is a critical autocrine growth factor as well as a mitogen for astrocytes, Schwann cells, and fibroblasts. It is ligand for epidermal growth factor (EGF) and it is related to transforming growth factor alpha (TGF-alpha). This protein interacts with the Epidermal growth factor receptor (EGFR) to promote the growth of normal epithelial cells.
Biological role
AREG is a critical factor in estrogen action and ductal development of the mammary glands.[9][10][11][12][13] Amphiregulin has been found to be essential for mammary ductal development, as evidenced by absence of ductal growth in amphiregulin knockout mice.[12] This is similar to the phenotypes of EGFR and ERα knockout mice, which also show absence of ductal growth.[12] Amphiregulin is expressed in many parts of body such as ovaries, placenta, pancreas, breasts, lungs and spleen. Expression of amphiregulin can be induced by TGF-α, TNF-α, interleukin 1, and prostaglandins.[14][15]
Clinical significance
Role in tissue repair
Generally, amphiregulin is considered to be a part of type 2 mediated resistance and tolerance, the latter of which occurs by promoting the reestablishment of tissue integrity after damage that is due to acute or chronic inflammation. Its involvement in tissue repair can be explained by its dual role, as amphiregulin can induce mitogenic signals, but it can also lead to cell differentiation of epithelial cells.[16]
While epithelial-derived amphiregulin can promote tissue repair, several immune cells are found to express it in cases of tissue damage, so amphiregulin is part of the crosstalk between immune and epithelial cells. [16][17]
A population of immune cells that is found to increase its amphiregulin expression after tissue damage, is the innate lymphoid cell 2 (ILC2) population. This has been observed in several organs, such as the lung, the intestine, and the skin. The expression of amphiregulin by ILC2s can be induced by interleukin 33 (IL-33).[18] Also, in skin derived ILC2s, amphiregulin expression was regulated by the interaction of killer-cell lectin-like receptor G1 (KLRG1) with E-cadherin.[19] After intestinal damage, activated intestinal ILC2s produce amphiregulin which enhances the production of mucin by epithelial cells, increases the expression of Claudin-1 and promotes the activity of goblet cells. These functions of amphiregulin lead to increased junction strength, as well as the strengthening of the mucus layer.[18]
Tissue resident regulatory T cells (Tregs) can also express amphiregulin to promote tissue repair. In the skeletal muscle, the IL-33 receptor (ST2) expressing Tregs have a distinct T-cell receptor (TCR) repertoire,[20] and TCR signals don’t seem to be required for amphiregulin production, but this process can be dependent on the IL-33/ST2 (or IL-33 receptor) pathway and the expression of interleukin 18 receptor (IL-18R) on tissue resident Tregs.[21] Also, amphiregulin that is expressed from these Tregs can further enhance their function, forming an autocrine positive feedback loop.[22] Amphiregulin-expressing tissue resident Tregs have been observed in the lung, where most of them are CD44hiCD62Llo and they express higher levels of CD103, programmed cell death protein 1 (PD-1), glucocorticoid-induced TNFR-related protein (GITR), cytotoxic T-lymphocyte antigen 4 (CTLA-4) and KLRG1.[21] They have been found in injured muscles, where this population has been associated with eosinophil influx, and the production of amphiregulin could enhance the colony-forming efficiency and myogenic differentiation of skeletal muscle satellite cells in vitro, increasing muscle healing.[16] In the inflamed colon, Gata3+Helios+ Tregs express high levels of amphiregulin too.[23] Moreover, Tregs that express amphiregulin, along with keratinocyte growth factor (KGF), CD39 and CD73, act on parenchymal cells to promote tissue repair and regeneration.[21]
Some unconventional T cells have been associated with the promotion of tissue repair by amphiregulin in a direct or in an indirect manner. After intestinal damage, mucosal-associated invariant T (MAIT) cells produce amphiregulin that leads to epithelial cell turnover and enhances the activity of goblet cells. Also, a pro-repair response by amphiregulin produced by ILC2s and Tregs, that is dependent on IL-33 signaling, is induced by gamma delta (γδ) T cells that produce interleukin 17A (IL-17A). This correlation between IL-17A-producing γδ T cells and amphiregulin has been observed in the lungs and in the oral mucosa.[18]
Psoriasis
Mutations in this encoded protein are associated with a psoriasis-like skin phenotype.[24][5] Higher circulating levels of amphiregulin are associated with AGVHD progression.[25] [26][27]
Cancer
Overexpression of amphiregulin is connected with cancer of the breast, prostate, colon, pancreas, lung, spleen, and bladder.[28][29][12]
Rheumatoid arthritis
It seems that expression of AREG is connected with proliferation of fibroblasts and production of proinflammatory cytokines interleukin 8 and vascular endothelial growth factor (VEGF).[30]
Fibrosis
Chronic elevation of amphiregulin levels has been associated with fibrosis in several organs. ILC2s are drivers of liver, skin, and pulmonary fibrosis, and their expression of interleukin 13 (IL-13) and amphiregulin is implicated in this process.[16] Pathogenic memory Th2 cells that express amphiregulin are also involved in pulmonary fibrosis. Exposure to house dust mite leads to the increase of amphiregulin-expressing pathogenic memory Th2 cells. This increase might be related to the IL-33/ST2 signaling, as blocking this pathway causes less production of amphiregulin. The function of amphiregulin in airway fibrosis is related to eosinophils that express EGFR, in which amphiregulin binds to, resulting in the upregulation of inflammatory genes, including Spp1 that encodes osteopontin. The expression of osteopontin by eosinophils shapes the pathogenesis of pulmonary fibrosis.[31] Moreover, macrophage-derived amphiregulin is involved in the transforming growth factor beta (TGF-β)-induced fibrosis too, as it has been found to activate latent TGF-β through the activation of integrin-αV complex.[16] [32][33] In the liver, ongoing necrosis leads to the activation of hepatic ILC2s which release amphiregulin along with IL-13. The release of them activates the hepatic stellate cells that transform into myofibroblasts, and ultimately promotes liver fibrosis.[19]
Inflammation
Amphiregulin is part of cellular response type 2.[34] It was found that the cell source of amphiregulin is innate lymphoid cells 2 (ILC2) which are dependent on interleukin 33. ILC2 expressed amphiregulin after tissue damage of the intestines and activation by IL-33. Moreover, endogenous AREG with IL-33 decreased the intestinal inflammation in mice with normal count of T-lymphocytes and in deficient mice.[35]
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000109321 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000029378 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b c "Entrez Gene: AREG amphiregulin (schwannoma-derived growth factor)".
- ^ Shoyab M, Plowman GD, McDonald VL, Bradley JG, Todaro GJ (February 1989). "Structure and function of human amphiregulin: a member of the epidermal growth factor family". Science. 243 (4894 Pt 1): 1074–1076. Bibcode:1989Sci...243.1074S. doi:10.1126/science.2466334. PMID 2466334.
- ^ Plowman GD, Green JM, McDonald VL, Neubauer MG, Disteche CM, Todaro GJ, et al. (May 1990). "The amphiregulin gene encodes a novel epidermal growth factor-related protein with tumor-inhibitory activity". Molecular and Cellular Biology. 10 (5): 1969–1981. doi:10.1128/MCB.10.5.1969. PMC 360543. PMID 2325643.
- ^ "AREG (amphiregulin (schwannoma-derived growth factor))". atlasgeneticsoncology.org. Archived from the original on 2019-08-27. Retrieved 2019-08-27.
- ^ Aupperlee MD, Leipprandt JR, Bennett JM, Schwartz RC, Haslam SZ (May 2013). "Amphiregulin mediates progesterone-induced mammary ductal development during puberty". Breast Cancer Research. 15 (3): R44. doi:10.1186/bcr3431. PMC 3738150. PMID 23705924.
- ^ LaMarca HL, Rosen JM (2007). "Estrogen regulation of mammary gland development and breast cancer: amphiregulin takes center stage". Breast Cancer Research. 9 (4): 304. doi:10.1186/bcr1740. PMC 2206713. PMID 17659070.
- ^ Kariagina A, Xie J, Leipprandt JR, Haslam SZ (October 2010). "Amphiregulin mediates estrogen, progesterone, and EGFR signaling in the normal rat mammary gland and in hormone-dependent rat mammary cancers". Hormones & Cancer. 1 (5): 229–244. doi:10.1007/s12672-010-0048-0. PMC 3000471. PMID 21258428.
- ^ a b c d McBryan J, Howlin J, Napoletano S, Martin F (June 2008). "Amphiregulin: role in mammary gland development and breast cancer". Journal of Mammary Gland Biology and Neoplasia. 13 (2): 159–169. doi:10.1007/s10911-008-9075-7. PMID 18398673. S2CID 13229645.
- ^ Sternlicht MD, Sunnarborg SW (June 2008). "The ADAM17-amphiregulin-EGFR axis in mammary development and cancer". Journal of Mammary Gland Biology and Neoplasia. 13 (2): 181–194. doi:10.1007/s10911-008-9084-6. PMC 2723838. PMID 18470483.
- ^ "AREG (amphiregulin (schwannoma-derived growth factor))". atlasgeneticsoncology.org. Archived from the original on 2019-08-27. Retrieved 2019-08-27.
- ^ Busser B, Sancey L, Brambilla E, Coll JL, Hurbin A (December 2011). "The multiple roles of amphiregulin in human cancer". Biochimica et Biophysica Acta (BBA) - Reviews on Cancer. 1816 (2): 119–131. doi:10.1016/j.bbcan.2011.05.003. PMID 21658434.
- ^ a b c d e Zaiss DM, Gause WC, Osborne LC, Artis D (February 2015). "Emerging functions of amphiregulin in orchestrating immunity, inflammation, and tissue repair". Immunity. 42 (2): 216–226. doi:10.1016/j.immuni.2015.01.020. PMC 4792035. PMID 25692699.
- ^ Singh SS, Chauhan SB, Kumar A, Kumar S, Engwerda CR, Sundar S, et al. (February 2022). "Amphiregulin in cellular physiology, health, and disease: Potential use as a biomarker and therapeutic target". Journal of Cellular Physiology. 237 (2): 1143–1156. doi:10.1002/jcp.30615. PMID 34698381. S2CID 239889516.
- ^ a b c Cox JR, Cruickshank SM, Saunders AE (2021). "Maintenance of Barrier Tissue Integrity by Unconventional Lymphocytes". Frontiers in Immunology. 12: 670471. doi:10.3389/fimmu.2021.670471. PMC 8079635. PMID 33936115.
- ^ a b Ochel A, Tiegs G, Neumann K (April 2019). "Type 2 Innate Lymphoid Cells in Liver and Gut: From Current Knowledge to Future Perspectives". International Journal of Molecular Sciences. 20 (8): 1896. doi:10.3390/ijms20081896. PMC 6514972. PMID 30999584.
- ^ Burzyn D, Kuswanto W, Kolodin D, Shadrach JL, Cerletti M, Jang Y, et al. (2013-12-05). "A special population of regulatory T cells potentiates muscle repair". Cell. 155 (6): 1282–1295. doi:10.1016/j.cell.2013.10.054. ISSN 1097-4172. PMC 3894749. PMID 24315098.
- ^ a b c Zhang C, Li L, Feng K, Fan D, Xue W, Lu J (2017-10-25). "'Repair' Treg Cells in Tissue Injury". Cellular Physiology and Biochemistry. 43 (6): 2155–2169. doi:10.1159/000484295. PMID 29069643.
- ^ Boothby IC, Cohen JN, Rosenblum MD (May 2020). "Regulatory T cells in skin injury: At the crossroads of tolerance and tissue repair". Science Immunology. 5 (47). doi:10.1126/sciimmunol.aaz9631. PMC 7274208. PMID 32358172.
- ^ Ito M, Komai K, Nakamura T, Srirat T, Yoshimura A (May 2019). "Tissue regulatory T cells and neural repair". International Immunology. 31 (6): 361–369. doi:10.1093/intimm/dxz031. PMID 30893423.
- ^ Bhagavathula N, Nerusu KC, Fisher GJ, Liu G, Thakur AB, Gemmell L, et al. (April 2005). "Amphiregulin and epidermal hyperplasia: amphiregulin is required to maintain the psoriatic phenotype of human skin grafts on severe combined immunodeficient mice". The American Journal of Pathology. 166 (4): 1009–1016. doi:10.1016/S0002-9440(10)62322-X. PMC 1780140. PMID 15793282.
- ^ Bhagavathula N, Nerusu KC, Fisher GJ, Liu G, Thakur AB, Gemmell L, et al. (April 2005). "Amphiregulin and epidermal hyperplasia: amphiregulin is required to maintain the psoriatic phenotype of human skin grafts on severe combined immunodeficient mice". The American Journal of Pathology. 166 (4): 1009–1016. doi:10.1016/S0002-9440(10)62322-X. PMC 1780140. PMID 15793282.
- ^ Holtan SG, DeFor TE, Panoskaltsis-Mortari A, Khera N, Levine JE, Flowers ME, et al. (August 2018). "Amphiregulin modifies the Minnesota Acute Graft-versus-Host Disease Risk Score: results from BMT CTN 0302/0802". Blood Advances. 2 (15): 1882–1888. doi:10.1182/bloodadvances.2018017343. PMC 6093743. PMID 30087106.
- ^ Piepkorn M (April 1996). "Overexpression of amphiregulin, a major autocrine growth factor for cultured human keratinocytes, in hyperproliferative skin diseases". The American Journal of Dermatopathology. 18 (2): 165–171. doi:10.1097/00000372-199604000-00010. PMID 8739992.
- ^ Busser B, Sancey L, Brambilla E, Coll JL, Hurbin A (December 2011). "The multiple roles of amphiregulin in human cancer". Biochimica et Biophysica Acta (BBA) - Reviews on Cancer. 1816 (2): 119–131. doi:10.1016/j.bbcan.2011.05.003. PMID 21658434.
- ^ "AREG (amphiregulin (schwannoma-derived growth factor))". atlasgeneticsoncology.org. Archived from the original on 2019-08-27. Retrieved 2019-08-27.
- ^ Yamane S, Ishida S, Hanamoto Y, Kumagai K, Masuda R, Tanaka K, et al. (April 2008). "Proinflammatory role of amphiregulin, an epidermal growth factor family member whose expression is augmented in rheumatoid arthritis patients". Journal of Inflammation. 5: 5. doi:10.1186/1476-9255-5-5. PMC 2396620. PMID 18439312.
- ^ Hirahara K, Aoki A, Morimoto Y, Kiuchi M, Okano M, Nakayama T (May 2019). "The immunopathology of lung fibrosis: amphiregulin-producing pathogenic memory T helper-2 cells control the airway fibrotic responses by inducing eosinophils to secrete osteopontin". Seminars in Immunopathology. 41 (3): 339–348. doi:10.1007/s00281-019-00735-6. PMID 30968186. S2CID 106409455.
- ^ Huang H, Yin K, Tang H (April 2020). "Macrophage amphiregulin-pericyte TGF-β axis: a novel mechanism of the immune system that contributes to wound repair". Acta Biochimica et Biophysica Sinica. 52 (4): 463–465. doi:10.1093/abbs/gmaa001. PMID 32147698.
- ^ Zaiss DM, Minutti CM, Knipper JA (July 2019). "Immune- and non-immune-mediated roles of regulatory T-cells during wound healing". Immunology. 157 (3): 190–197. doi:10.1111/imm.13057. PMC 6600083. PMID 30866049.
- ^ Zaiss DM, Yang L, Shah PR, Kobie JJ, Urban JF, Mosmann TR (December 2006). "Amphiregulin, a TH2 cytokine enhancing resistance to nematodes". Science. 314 (5806): 1746. Bibcode:2006Sci...314.1746Z. doi:10.1126/science.1133715. PMID 17170297. S2CID 27808704.
- ^ Monticelli LA, Osborne LC, Noti M, Tran SV, Zaiss DM, Artis D (August 2015). "IL-33 promotes an innate immune pathway of intestinal tissue protection dependent on amphiregulin-EGFR interactions". Proceedings of the National Academy of Sciences of the United States of America. 112 (34): 10762–10767. Bibcode:2015PNAS..11210762M. doi:10.1073/pnas.1509070112. PMC 4553775. PMID 26243875.
Further reading
- Culouscou JM, Remacle-Bonnet M, Carlton GW, Plowman GD, Shoyab M (1993). "Colorectum cell-derived growth factor (CRDGF) is homologous to amphiregulin, a member of the epidermal growth factor family". Growth Factors. 7 (3): 195–205. doi:10.3109/08977199209046924. PMID 1333777.
- Cook PW, Mattox PA, Keeble WW, Pittelkow MR, Plowman GD, Shoyab M, et al. (May 1991). "A heparin sulfate-regulated human keratinocyte autocrine factor is similar or identical to amphiregulin". Molecular and Cellular Biology. 11 (5): 2547–2557. doi:10.1128/MCB.11.5.2547. PMC 360024. PMID 2017164.
- Kimura H, Fischer WH, Schubert D (November 1990). "Structure, expression and function of a schwannoma-derived growth factor". Nature. 348 (6298): 257–260. Bibcode:1990Natur.348..257K. doi:10.1038/348257a0. PMID 2234093. S2CID 4275004.
- Plowman GD, Green JM, McDonald VL, Neubauer MG, Disteche CM, Todaro GJ, et al. (May 1990). "The amphiregulin gene encodes a novel epidermal growth factor-related protein with tumor-inhibitory activity". Molecular and Cellular Biology. 10 (5): 1969–1981. doi:10.1128/MCB.10.5.1969. PMC 360543. PMID 2325643.
- Shoyab M, Plowman GD, McDonald VL, Bradley JG, Todaro GJ (February 1989). "Structure and function of human amphiregulin: a member of the epidermal growth factor family". Science. 243 (4894 Pt 1): 1074–1076. Bibcode:1989Sci...243.1074S. doi:10.1126/science.2466334. PMID 2466334.
- Shoyab M, McDonald VL, Bradley JG, Todaro GJ (September 1988). "Amphiregulin: a bifunctional growth-modulating glycoprotein produced by the phorbol 12-myristate 13-acetate-treated human breast adenocarcinoma cell line MCF-7". Proceedings of the National Academy of Sciences of the United States of America. 85 (17): 6528–6532. Bibcode:1988PNAS...85.6528S. doi:10.1073/pnas.85.17.6528. PMC 282006. PMID 3413110.
- Chen CS, Bejcek BE, Kersey JH (1995). "A mapping study of 13 genes on human chromosome bands 4q11→q25". Cytogenetics and Cell Genetics. 69 (3–4): 260–265. doi:10.1159/000133976. PMID 7698025.
- Cook PW, Piepkorn M, Clegg CH, Plowman GD, DeMay JM, Brown JR, et al. (November 1997). "Transgenic expression of the human amphiregulin gene induces a psoriasis-like phenotype". The Journal of Clinical Investigation. 100 (9): 2286–2294. doi:10.1172/JCI119766. PMC 508424. PMID 9410906.
- Wong L, Deb TB, Thompson SA, Wells A, Johnson GR (March 1999). "A differential requirement for the COOH-terminal region of the epidermal growth factor (EGF) receptor in amphiregulin and EGF mitogenic signaling". The Journal of Biological Chemistry. 274 (13): 8900–8909. doi:10.1074/jbc.274.13.8900. PMID 10085134.
- Reddy KB, Krueger JS, Kondapaka SB, Diglio CA (July 1999). "Mitogen-activated protein kinase (MAPK) regulates the expression of progelatinase B (MMP-9) in breast epithelial cells". International Journal of Cancer. 82 (2): 268–273. doi:10.1002/(SICI)1097-0215(19990719)82:2<268::AID-IJC18>3.0.CO;2-4. PMID 10389762. S2CID 22627041.
- Fernandes AM, Hamburger AW, Gerwin BI (July 1999). "Production of epidermal growth factor related ligands in tumorigenic and benign human lung epithelial cells". Cancer Letters. 142 (1): 55–63. doi:10.1016/S0304-3835(99)00166-4. PMID 10424781.
- Lee SB, Huang K, Palmer R, Truong VB, Herzlinger D, Kolquist KA, et al. (September 1999). "The Wilms tumor suppressor WT1 encodes a transcriptional activator of amphiregulin". Cell. 98 (5): 663–673. doi:10.1016/S0092-8674(00)80053-7. PMID 10490105. S2CID 14607182.
- Tokumaru S, Higashiyama S, Endo T, Nakagawa T, Miyagawa JI, Yamamori K, et al. (October 2000). "Ectodomain shedding of epidermal growth factor receptor ligands is required for keratinocyte migration in cutaneous wound healing". The Journal of Cell Biology. 151 (2): 209–220. doi:10.1083/jcb.151.2.209. PMC 2192647. PMID 11038170.
- Ebert MP, Hernberg S, Fei G, Sokolowski A, Schulz HU, Lippert H, et al. (July 2001). "Induction and expression of cyclin D3 in human pancreatic cancer". Journal of Cancer Research and Clinical Oncology. 127 (7): 449–454. doi:10.1007/s004320100235. PMID 11469683. S2CID 33146049.
- Berquin IM, Dziubinski ML, Nolan GP, Ethier SP (July 2001). "A functional screen for genes inducing epidermal growth factor autonomy of human mammary epithelial cells confirms the role of amphiregulin". Oncogene. 20 (30): 4019–4028. doi:10.1038/sj.onc.1204537. PMID 11494130.
- Thøgersen VB, Sørensen BS, Poulsen SS, Orntoft TF, Wolf H, Nexo E (August 2001). "A subclass of HER1 ligands are prognostic markers for survival in bladder cancer patients". Cancer Research. 61 (16): 6227–6233. PMID 11507076.
- Wolfgang CD, Essand M, Lee B, Pastan I (November 2001). "T-cell receptor gamma chain alternate reading frame protein (TARP) expression in prostate cancer cells leads to an increased growth rate and induction of caveolins and amphiregulin". Cancer Research. 61 (22): 8122–8126. PMID 11719440.
- Schiemann U, Konturek J, Assert R, Rembiasz K, Domschke W, Konturek S, et al. (February 2002). "mRNA expression of EGF receptor ligands in atrophic gastritis before and after Helicobacter pylori eradication". Medical Science Monitor. 8 (2): CR53–CR58. PMID 11859273.
- Tørring N, Møller-Ernst Jensen K, Lund L, Nielsen JE, Djurhuus JC, Poulsen SS, et al. (April 2002). "Possible autocrine loop of the epidermal growth factor system in patients with benign prostatic hyperplasia treated with finasteride: a placebo-controlled randomized study". BJU International. 89 (6): 583–590. doi:10.1046/j.1464-410X.2002.02665.x. PMID 11942969. S2CID 42241168.
- Hurbin A, Dubrez L, Coll JL, Favrot MC (December 2002). "Inhibition of apoptosis by amphiregulin via an insulin-like growth factor-1 receptor-dependent pathway in non-small cell lung cancer cell lines". The Journal of Biological Chemistry. 277 (51): 49127–49133. doi:10.1074/jbc.M207584200. PMID 12356750.
External links
- Human AR genome location and AR gene details page in the UCSC Genome Browser.
- Human AREG genome location and AREG gene details page in the UCSC Genome Browser.
- Overview of all the structural information available in the PDB for UniProt: P15514 (Amphiregulin) at the PDBe-KB.