Toxic megacolon
| Toxic megacolon | |
|---|---|
| Other names | Megacolon toxicum |
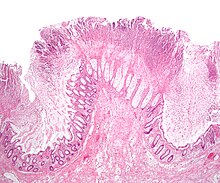 | |
| Micrograph of pseudomembranous colitis, a cause of toxic megacolon. H&E stain. | |
| Specialty | Gastroenterology |
| Symptoms | Swelling of the belly, Pain in the belly, Fever, Rapid heart rate, Shock, Diarrhea.[1] |
| Complications | Septic shock, perforation of the colon |
| Risk factors | Chronic bowel disease |
| Prognosis | Fatal without treatment |
Toxic megacolon is an acute form of colonic distension.[2] It is characterized by a very dilated colon (megacolon), accompanied by abdominal distension (bloating), and sometimes fever, abdominal pain, or shock.
Toxic megacolon is usually a complication of inflammatory bowel disease, such as ulcerative colitis and, more rarely, Crohn's disease, and of some infections of the colon, including Clostridioides difficile infections, which have led to pseudomembranous colitis. Other forms of megacolon exist and can be congenital (present since birth, such as Hirschsprung's disease). It can also be caused by Entamoeba histolytica and Shigella. It may also be caused by the use of loperamide.
Signs and symptoms
- Abdominal bloating
- Abdominal pain
- Abdominal tenderness
- Dehydration
- Fever
- Tachycardia (rapid heart rate)
There may be signs of septic shock. A physical examination reveals abdominal tenderness and possible loss of bowel sounds. An abdominal radiography shows colonic dilation. White blood cell count is usually elevated. Severe sepsis may present with hypothermia or leukopenia.[citation needed]
Complications
- Perforation of the colon[3]
- Sepsis
- Shock
Emergency action may be required if severe abdominal pain develops, particularly if it is accompanied by fever, rapid heart rate, tenderness when the abdomen is pressed, bloody diarrhea, frequent diarrhea, or painful bowel movements.
Colonoscopy is contraindicated, as it may rupture the dilated colon resulting in peritonitis and septic shock.
Pathophysiology


The pathological process involves inflammation and damage to the colonic wall with unknown toxins breaking down the protective mucosal barrier and exposing the muscularis propria.[4] There is relative destruction of the ganglion cells and swelling of the nerve fibers in the myenteric plexus, with concomitant damage to the colonic musculature.[4] This results in almost complete paralysis of the diseased segment of the colon with loss of smooth muscle substance, tone and motility.[4] This can lead to further complications as pressure builds up in the colon due to relative fecal stasis including sepsis, intestinal hemorrhage or free perforation and spontaneous decompression.[4]
Diagnosis
Massively dilated colon with air-fluid level can be seen on abdominal radiograph or CT scan.[5][6]
Treatment
The objective of treatment is to decompress the bowel and to prevent swallowed air from further distending the bowel. If decompression is not achieved or the patient does not improve with medical management, surgery is indicated. When surgery is required the recommended procedure is a colectomy (surgical removal of all or part of the colon) with end ileostomy.[7] Fluid and electrolyte replacement help to prevent dehydration and shock. Use of corticosteroids may be indicated to suppress the inflammatory reaction in the colon if megacolon has resulted from active inflammatory bowel disease. Antibiotics may be given to prevent sepsis.[8]
Prognosis
If the condition does not improve, the risk of death is significant. In case of poor response to conservative therapy, a colectomy is usually required.[9]
References
- ^ "Toxic Megacolon". Johns Hopkins Medicine. 19 November 2019. Retrieved 15 March 2023.
- ^ "Toxic megacolon" at Dorland's Medical Dictionary
- ^ Panos, MZ; Wood, MJ; Asquith, P (December 1993). "Toxic megacolon: The knee-elbow position relieves bowel distension". Gut. 34 (12): 1726–7. doi:10.1136/gut.34.12.1726. PMC 1374472. PMID 8282262.
- ^ a b c d Michael B; et al. (1980). "Toxic megacolon complicating Crohn's Colitis". Ann. Surg. 191 (1): 75–80. doi:10.1097/00000658-198001000-00015. PMC 1344622. PMID 7352781.
- ^ "Toxic megacolon: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2022-11-18.
- ^ "Toxic megacolon httpsmedlineplus.govencyarticle000248.htm". profilpelajar.com. Retrieved 2022-11-18.
- ^ Seltman, AK (December 2012). "Surgical Management of Clostridium difficile Colitis". Clinics in Colon and Rectal Surgery. 25 (4): 204–9. doi:10.1055/s-0032-1329390. PMC 3577611. PMID 24294121.
- ^ Autenrieth, DM; Baumgart, DC (August 2011). "Toxic megacolon". Inflammatory Bowel Diseases. 18 (3): 584–91. doi:10.1002/ibd.21847. PMID 22009735. S2CID 32866477.
- ^ Benchimol, EI; Turner, D; Mann, EH; Thomas, KE; et al. (June 2008). "Toxic megacolon in children with inflammatory bowel disease: Clinical and radiographic characteristics". The American Journal of Gastroenterology. 103 (6): 1524–31. doi:10.1111/j.1572-0241.2008.01807.x. PMID 18510624. S2CID 23729183.
- This article incorporates text from the United States National Library of Medicine (Toxic megacolon), which is in the public domain.
Further reading
- Ausch, C; Madoff, RD; Gnant, M; Rosen, HR; Garcia-Aguilar, J; Hölbling, N; Herbst, F; Buxhofer, V; Holzer, B; Rothenberger, DA; Schiessel, R (March 2006). "Aetiology and surgical management of toxic megacolon". Colorectal Disease. 8 (3): 195–201. doi:10.1111/j.1463-1318.2005.00887.x. PMID 16466559. S2CID 36384160.
- Toxic Megacolon at eMedicine
