Oral mucocele
| Mucous cyst of the oral mucocele | |
|---|---|
 | |
| A mucocele on the lower lip. | |
| Specialty | Oral and maxillofacial surgery |
Oral mucocele (also mucous extravasation cyst, mucous cyst of the oral mucosa,[1] and mucous retention and extravasation phenomena) is a condition caused by two related phenomena - mucus extravasation phenomenon and mucous retention cyst.
Mucous extravasation phenomenon is a swelling of connective tissue consisting of a collection of fluid called mucus. This occurs because of a ruptured salivary gland duct usually caused by local trauma (damage) in the case of mucous extravasation phenomenon and an obstructed or ruptured salivary duct in the case of a mucus retention cyst. The mucocele has a bluish, translucent color, and is more commonly found in children and young adults.
Although these lesions are often called cysts, mucoceles are not true cysts because they have no epithelial lining.[2] Rather, they are polyps.[3]
Signs and symptoms
The size of oral mucoceles vary from 1 mm to several centimeters and they usually are slightly transparent with a blue tinge. On palpation, mucoceles may appear fluctuant, but can also be firm. Their duration lasts from days to years,[4] and may have recurrent swelling with occasional rupturing of its contents.

Locations
The most common location to find a mucocele is the inner surface of the lower lip. It can also be found on the inner side of the cheek (known as the buccal mucosa), on the anterior ventral tongue, and the floor of the mouth. When found on the floor of the mouth, the mucocele is referred to as a ranula. They are rarely found on the upper lip. As their name suggests, they are basically mucus-lined cysts and they can also occur in the paranasal sinuses, most commonly the frontal sinuses, the frontoethmoidal region, and the maxillary sinus. Sphenoid sinus involvement is extremely rare. When the lumen of the vermiform appendix of the intestine gets blocked due to any factor, a mucocele can also form there.
Variations
A variant of a mucocele is found on the palate, retromolar pad, and posterior buccal mucosa. Known as a "superficial mucocele", this type presents as single or multiple vesicles and bursts into an ulcer. Despite healing after a few days, superficial mucoceles recur often in the same location. Other causes of bumps inside lips are aphthous ulcer, lipoma, benign tumors of salivary glands, submucous abscesses, and haemangiomas.
Diagnosis

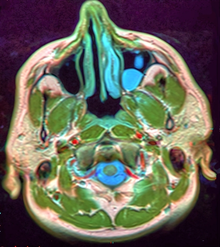
Microscopically, mucoceles appears as granulation tissue surrounding mucin. Since inflammation occurs concurrently, neutrophils and foamy histiocytes usually are present. On a CT scan, a mucocele is fairly homogenous, with an attenuation of about 10-18 Hounsfield units.[5]
Classification
Both mucous retention and extravasation phenomena are classified as salivary gland disorders.
Treatment

Some mucoceles spontaneously resolve on their own after a short time. Others are chronic and require surgical removal. Recurrence is possible, thus the adjacent salivary gland may be excised as a preventive measure. Hence surgical removal of cyst is treatment of choice.[7]
Several types of procedures are available for the surgical removal of mucoceles. These include laser and minimally invasive techniques, which means recovery times are reduced drastically.[8]
Micromarsupialization is an alternative procedure to surgical removal. It uses silk sutures in the dome of a cyst to allow new epithelialized drainage pathways. It is simpler, less traumatic, and well tolerated by patients, especially children.[9]
A nonsurgical option that may be effective for a small or newly identified mucocele is to rinse the mouth thoroughly with salt water (one tablespoon of salt per cup) four to six times a day for a few days. This may draw out the fluid trapped underneath the skin without further damaging the surrounding tissue.[10] If the mucocele persists, individuals should see a doctor to discuss further treatment. Smaller cysts may be removed by laser treatment, but larger cysts may have to be removed surgically.[citation needed]
See also
References
- ^ Rapini RP, Bolognia JL, Jorizzo JL (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- ^ Mucocele at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- ^ "Dorlands Medical Dictionary:mucocele". Archived from the original on 2009-11-14.
- ^ Sinha R, Sarkar S, Khaitan T, Kabiraj A, Maji A (2016). "Nonsurgical Management of Oral Mucocele by Intralesional Corticosteroid Therapy". International Journal of Dentistry. 2016: 2896748. doi:10.1155/2016/2896748. PMC 5086369. PMID 27822227.
- ^ page 152 in: Luca Saba and Jasjit S. Suri (2013). Multi-Detector CT Imaging: Principles, Head, Neck, and Vascular Systems. CRC Press. ISBN 9781439893845.
- ^ Dorfman J. "The Center for Special Dentistry".
- ^ Nallasivam, K. U.; Sudha, B. R. (2015). "Oral mucocele: Review of literature and a case report". Journal of Pharmacy & Bioallied Sciences. 7 (Suppl 2): S731–733. doi:10.4103/0975-7406.163516. ISSN 0976-4879. PMC 4606697. PMID 26538955.
- ^ Bagher, Sara M.; Sulimany, Ayman M.; Kaplan, Martin; Loo, Cheen Y. (9 May 2018). "Treating Mucocele in Pediatric Patients Using a Diode Laser: Three Case Reports". Dentistry Journal. 6 (2): 13. doi:10.3390/dj6020013. PMC 6023325. PMID 29747378.
- ^ Piazzetta CM, Torres-Pereira C, Amenábar JM (September 2012). "Micro-marsupialization as an alternative treatment for mucocele in pediatric dentistry". International Journal of Paediatric Dentistry. 22 (5): 318–23. doi:10.1111/j.1365-263X.2011.01198.x. PMID 22092694.
- ^ DoctorGentry (2016-08-13). "mucocele | Dr. Gentry". Retrieved 2024-03-23.
