Creatine transporter defect
| Creatine transporter defect | |
|---|---|
 | |
| Specialty | Medical genetics |
| Causes | Deficiency of creatine transporter |
| Diagnostic method | Genetic testing, magnetic resonance spectroscopy, blood and urine testing |
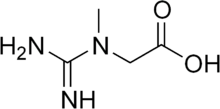
Creatine transporter deficiency (CTD) is an inborn error of creatine metabolism in which creatine is not properly transported to the brain and muscles due to defective creatine transporters. CTD is an X-linked disorder caused by mutation in SLC6A8. SLC6A8 is located at Xq28.[1] Hemizygous males with CTD express speech and behavior abnormalities, intellectual disabilities, development delay, seizures, and autistic behavior. Heterozygous females with CTD generally express fewer, less severe symptoms.[1][2][3] CTD is one of three different types of cerebral creatine deficiency (CCD). The other two types of CCD are guanidinoacetate methyltransferase (GAMT) deficiency and L-arginine:glycine amidinotransferase (AGAT) deficiency. Clinical presentation of CTD is similar to that of GAMT and AGAT deficiency.[4][1] CTD was first identified in 2001 with the presence of a hemizygous nonsense change in SLC6A8 in a male patient.[1]
Signs and symptoms
Generally, the majority of individuals with creatine transporter defect express the following symptoms with varying levels of severity: developmental delay and regression, intellectual disability, and abnormalities in expressive and cognitive speech.[5] However, several studies have shown a wider variety of symptoms including, but not limited to attention deficit and hyperactivity with impulsivity, myopathy, hypotonia, semantic-pragmatic language disorder, oral dyspraxia, extrapyramidal movement disorder, constipation, absent speech development, seizures, and epilepsy.[6][2][3][7] Furthermore, symptoms can significantly vary between hemizygous males and heterozygous females, although, symptoms are generally more severe in hemizygous males. Hemizygous males more commonly express seizures, growth deficiency, severe intellectual disability, and severe expressive language impairment.[2][3] Heterozygous females more commonly express mild intellectual disability, impairments to confrontational naming and verbal memory, and learning and behavior problems.[6][2][8]
Genetics
CTD is caused by pathogenic variants in SLC6A8, located at Xq28. Over 60 variants in SLC6A8 have been reported.[9] SLC6A8 contains 13 exons and spreads across 8.5 kb of genomic DNA (gDNA).[10] The presence of hemizygous variants in males and heterozygous variants in females in SLC6A8 provides evidence that CTD is inherited in an X-linked recessive manner. This usually results in hemizygous males having severe symptoms, while heterozygous female carriers tend to have less severe and more varying symptoms.[7][8]
Mechanism
The creatine phosphate system is needed for the storage and transmission of phosphate-bound energy in the brain and muscle. The brain and muscle have particularly high metabolic demands, therefore, making creatine a necessary molecule in ATP homeostasis.[11][12] In regard to the brain, in order for creatine to reach the brain, it must first pass through the blood–brain barrier (BBB). The BBB separates blood from brain interstitial fluid and is, therefore, able to regulate the transfer of nutrients to the brain from the blood. In order to pass through the BBB, creatine utilizes creatine transporter (CRT). When present at the BBB, CRT mediates the passage of creatine from the blood to the brain. When being transported from the blood to the brain, creatine has to constantly move against the creatine concentration gradient that is present at the border between the brain and circulating blood.[13]
Diagnosis
The diagnosis of CTD is usually suspected based on the clinical presentation of intellectual disability, abnormalities in cognitive and expressive speech, and developmental delay. Furthermore, a family history of X-linked intellectual disability, developmental coordination disorder, and seizures is strongly suggestive.[14] Initial screening of CTD involves obtaining a urine sample and measuring the ratio of creatine to creatinine. If the ratio of creatine to creatinine is greater than 1.5, then the presence of CTD is highly likely. This is because a large ratio indicates a high amount of creatine in the urine.[7][15] This, in turn, indicates inadequate transport of creatine into the brain and muscle. However, the urine screening test often fails in diagnosing heterozygous females. Studies have demonstrated that as a group heterozygous females have significantly decreased cerebral creatine concentration, but that individual heterozygous females often have normal creatine concentrations found in their urine. Therefore, urine screening tests are unreliable as a standard test for diagnosing CTD, particularly in females.[8]
A more reliable and sophisticated manner of testing for cerebral creatine concentrations is through in vivo proton magnetic resonance spectroscopy (1H MRS). In vivo 1H MRS uses proton signals to determine the concentration of specific metabolites. This method of testing is more reliable because it provides a fairly accurate measurement of the amount of creatine inside the brain. Similar to urine testing, a drawback of using 1H MRS as a test for CTD is that the results of the test could be attributed to any of the cerebral creatine deficiencies.[15] The most accurate and reliable method of testing for CTD is through DNA sequence analysis of SLC6A8. DNA analysis of SLC6A8 allows the identification of the location and type of variant causing the cerebral creatine deficiency. Furthermore, DNA analysis of SLC6A8 is able to prove that a cerebral creatine deficiency is due to CTD and not GAMT or AGAT deficiency.[4][7][8]
Treatment
CTD is difficult to treat because the actual transporter responsible for transporting creatine to the brain and muscles is defective. Affected individuals have sufficient amounts of creatine, however it cannot get to the tissues where it is needed. Studies in which oral creatine monohydrate supplements were given to patients with CTD found that patients did not respond to treatment. However, similar studies conducted in which patients that had GAMT or AGAT deficiency were given oral creatine monohydrate supplements found that patient's clinical symptoms improved. Patients with CTD are unresponsive to oral creatine monohydrate supplements because regardless of the amount of creatine they ingest, the creatine transporter is still defective, and therefore creatine is incapable of being transported across the BBB.[15][16] Given the major role that the BBB has in the transport of creatine to the brain and unresponsiveness of oral creatine monohydrate supplements in CTD patients, future research will focus on working with the BBB to deliver creatine supplements.[13] However, given the limited number of patients that have been identified with CTD, future treatment strategies must be more effective and efficient when recognizing individuals with CTD.[1][15]
Patient Support
There are two organizations that support patients and families affected by Creatine Transporter Defect (CTD). The international organization, Association for Creatine Deficiencies (ACD), supports patients with all three Cerebral Creatine Deficiency Syndromes (CCDS), including AGAT Deficiency, GAMT Deficiency, and CTD. Their mission is to advance education, diagnosis, and research of CCDS. ACD's website is creatineinfo.org. The French organization, Xtraordinaire, represents families with relatives with mental retardation linked to the X chromosome, including CTD. Xtraordinaire's website is xtraordinaire.org.
References
- ^ a b c d e Salomons, G. S.; Dooren, S. J. M. Van; Verhoeven, N. M.; Marsden, D.; Schwartz, C.; Cecil, K. M.; DeGrauw, T. J.; Jakobs, C. (2003). "X-linked creatine transporter defect: An overview". Journal of Inherited Metabolic Disease. 26 (2–3): 309–318. doi:10.1023/A:1024405821638. ISSN 0141-8955. PMID 12889669. S2CID 7062586.
- ^ a b c d Hahn, Kimberly A.; Salomons, Gajja S.; Tackels-Horne, Darci; Wood, Tim C.; Taylor, Harold A.; Schroer, Richard J.; Lubs, Herbert A.; Jakobs, Cornelis; Olson, Rick L. (2002). "X-Linked Mental Retardation with Seizures and Carrier Manifestations Is Caused by a Mutation in the Creatine-Transporter Gene (SLC6A8) Located in Xq28". The American Journal of Human Genetics. 70 (5): 1349–1356. doi:10.1086/340092. PMC 447610. PMID 11898126.
- ^ a b c Anselm, I. M.; Alkuraya, F. S.; Salomons, G. S.; Jakobs, C.; Fulton, A. B.; Mazumdar, M.; Rivkin, M.; Frye, R.; Poussaint, T. Young (2006). "X-linked creatine transporter defect: A report on two unrelated boys with a severe clinical phenotype". Journal of Inherited Metabolic Disease. 29 (1): 214–219. doi:10.1007/s10545-006-0123-4. ISSN 0141-8955. PMC 2393549. PMID 16601897.
- ^ a b "OMIM Entry - # 300352 - CEREBRAL CREATINE DEFICIENCY SYNDROME 1; CCDS1". www.omim.org. Retrieved 2016-11-27.
- ^ Schulze, Andreas (2003-01-01). "Creatine deficiency syndromes". In Clark, Joseph F. (ed.). Guanidino Compounds in Biology and Medicine. Molecular and Cellular Biochemistry. Springer US. pp. 143–150. doi:10.1007/978-1-4615-0247-0_22. ISBN 9781461349853.
- ^ a b deGrauw, Ton J.; Cecil, Kim M.; Byars, Anna W.; Salomons, Gajja S.; Ball, William S.; Jakobs, Cornelis (2003-01-01). Clark, Joseph F. (ed.). Guanidino Compounds in Biology and Medicine. Molecular and Cellular Biochemistry. Springer US. pp. 45–48. doi:10.1007/978-1-4615-0247-0_6. ISBN 9781461349853.
- ^ a b c d Mancini, G.m.s.; Catsman-Berrevoets, C.e.; de Coo, I.f.m.; Aarsen, F.k.; Kamphoven, J.h.j.; Huijmans, J.g.; Duran, M.; van der Knaap, M.s.; Jakobs, C. (2005-01-30). "Two novel mutations in SLC6A8 cause creatine transporter defect and distinctive X-linked mental retardation in two unrelated Dutch families". American Journal of Medical Genetics Part A. 132A (3): 288–295. doi:10.1002/ajmg.a.30473. ISSN 1552-4833. PMID 15690373. S2CID 12694913.
- ^ a b c d van de Kamp, Jm; Mancini, Gms; Pouwels, Pjw; Betsalel, Ot; van Dooren, Sjm; de Koning, I; Steenweg, Me; Jakobs, C; van der Knaap, Ms (2011-03-01). "Clinical features and X-inactivation in females heterozygous for creatine transporter defect". Clinical Genetics. 79 (3): 264–272. doi:10.1111/j.1399-0004.2010.01460.x. ISSN 1399-0004. PMID 20528887. S2CID 6514503.
- ^ Goldstein, Jennifer; Thomas-Wilson, Amanda; Groopman, Emily; Aggarwal, Vimla; Bianconi, Simona; Fernandez, Raquel; Hart, Kim; Longo, Nicola; Liang, Nicole; Reich, Daniel; Wallis, Heidi; Weaver, Meredith; Young, Sarah; Mercimek-Andrews, Saadet (May 2024). "ClinGen variant curation expert panel recommendations for classification of variants in GAMT, GATM and SLC6A8 for cerebral creatine deficiency syndromes". Molecular Genetics and Metabolism. 142 (1): 108362. doi:10.1016/j.ymgme.2024.108362. ISSN 1096-7206. PMID 38452609.
- ^ Sandoval, Natalia; Bauer, David; Brenner, Volker; Coy, Johannes F.; Drescher, Bernd; Kioschis, Petra; Korn, Bernd; Nyakatura, Gerald; Poustka, Annemarie (1996-07-15). "The Genomic Organization of a Human Creatine Transporter (CRTR) Gene Located in Xq28". Genomics. 35 (2): 383–385. doi:10.1006/geno.1996.0373. PMID 8661155.
- ^ Snow, Rodney J.; Murphy, Robyn M. (2001). "Creatine and the creatine transporter: A review". Molecular and Cellular Biochemistry. 224 (1–2): 169–181. doi:10.1023/A:1011908606819. ISSN 0300-8177. PMID 11693194. S2CID 28502746.
- ^ Stöckler, Sylvia; Hanefeld, Folker; Frahm, Jens (1996). "Creatine replacement therapy in guanidineoacetate methyltransferase deficiency, a novel inborn error of metabolism". The Lancet. 348 (9030): 789–790. doi:10.1016/s0140-6736(96)04116-5. PMID 8813986. S2CID 31345881.
- ^ a b Ohtsuki, Sumio; Tachikawa, Masanori; Takanaga, Hitomi; Shimizu, Hidemi; Watanabe, Masahiko; Hosoya, Ken-ichi; Terasaki, Tetsuya (2002-11-01). "The Blood–Brain Barrier Creatine Transporter is a Major Pathway for Supplying Creatine to the Brain". Journal of Cerebral Blood Flow & Metabolism. 22 (11): 1327–1335. doi:10.1097/01.WCB.0000033966.83623.7D. ISSN 0271-678X. PMID 12439290.
- ^ Leuzzi, Vincenzo; Mastrangelo, Mario; Battini, Roberta; Cioni, Giovanni (2013-02-01). "Inborn errors of creatine metabolism and epilepsy". Epilepsia. 54 (2): 217–227. doi:10.1111/epi.12020. ISSN 1528-1167. PMID 23157605. S2CID 19842465.
- ^ a b c d Stromberger, C.; Bodamer, O. A.; Stöckler-Ipsiroglu, S. (2003). "Clinical characteristics and diagnostic clues in inborn errors of creatine metabolism". Journal of Inherited Metabolic Disease. 26 (2–3): 299–308. doi:10.1023/A:1024453704800. ISSN 0141-8955. PMID 12889668. S2CID 24963392.
- ^ Wyss, Markus; Schulze, Andreas (2002-06-18). "Health implications of creatine: can oral creatine supplementation protect against neurological and atherosclerotic disease?". Neuroscience. 112 (2): 243–260. doi:10.1016/S0306-4522(02)00088-X. PMID 12044443. S2CID 24582378.
