Blood sugar regulation
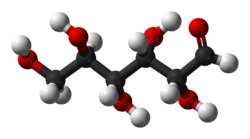
Blood sugar regulation is the process by which the levels of blood sugar, the common name for glucose dissolved in blood plasma, are maintained by the body within a narrow range.

This tight regulation is referred to as glucose homeostasis. Insulin, which lowers blood sugar, and glucagon, which raises it, are the most well known of the hormones involved, but more recent discoveries of other glucoregulatory hormones have expanded the understanding of this process. The gland called pancreas secretes two hormones and they are primarily responsible to regulate glucose levels in blood.[1]
Mechanisms

Blood sugar levels are regulated by negative feedback in order to keep the body in balance.[2][3][4][5] The levels of glucose in the blood are monitored by many tissues, but the cells in the pancreatic islets are among the most well understood and important.[citation needed]
Granule docking is an important glucose-dependent step in human insulin secretion that does not work properly in type 2 diabetes.[6]
Glucagon
If the blood glucose level falls to dangerously low levels (as during very heavy exercise or lack of food for extended periods), the alpha cells of the pancreas release glucagon, a peptide hormone which travels through the blood to the liver, where it binds to glucagon receptors on the surface of liver cells and stimulates them to break down glycogen stored inside the cells into glucose (this process is called glycogenolysis). The cells release the glucose into the bloodstream, increasing blood sugar levels. Hypoglycemia, the state of having low blood sugar, is treated by restoring the blood glucose level to normal by the ingestion or administration of dextrose or carbohydrate foods. It is often self-diagnosed and self-medicated orally by the ingestion of balanced meals. In more severe circumstances, it is treated by injection or infusion of glucagon.[citation needed]
Insulin
When levels of blood sugar rise, whether as a result of glycogen conversion, or from digestion of a meal, a different hormone is released from beta cells found in the islets of Langerhans in the pancreas. This hormone, insulin, causes the liver to convert more glucose into glycogen (this process is called glycogenesis), and to force about 2/3 of body cells (primarily muscle and fat tissue cells) to take up glucose from the blood through the GLUT4 transporter, thus decreasing blood sugar. When insulin binds to the receptors on the cell surface, vesicles containing the GLUT4 transporters come to the plasma membrane and fuse together by the process of endocytosis, thus enabling a facilitated diffusion of glucose into the cell. As soon as the glucose enters the cell, it is phosphorylated into glucose-6-phosphate in order to preserve the concentration gradient so glucose will continue to enter the cell.[7] Insulin also provides signals to several other body systems, and is the chief regulator of metabolic control in humans.[citation needed]
There are also several other causes for an increase in blood sugar levels. Among them are the 'stress' hormones such as epinephrine (also known as adrenaline), several of the steroids, infections, trauma, and of course, the ingestion of food.[citation needed]
Diabetes mellitus type 1 is caused by insufficient or non-existent production of insulin, while type 2 is primarily due to a decreased response to insulin in the tissues of the body (insulin resistance). Both types of diabetes, if untreated, result in too much glucose remaining in the blood (hyperglycemia) and many of the same complications. Also, too much insulin and/or exercise without enough corresponding food intake in diabetics can result in low blood sugar (hypoglycemia).[citation needed]
Hormones that influence blood glucose level
| Hormone | Tissue of origin | Metabolic effect | Effect on blood glucose |
|---|---|---|---|
| Insulin | Pancreatic β Cells | 1) Enhances entry of glucose into cells; 2) Enhances storage of glucose as glycogen, or conversion to fatty acids; 3) Enhances synthesis of fatty acids and proteins; 4) Suppresses breakdown of proteins into amino acids, and Triglycerides (from adipose tissue) into free fatty acids. | Lowers |
| Amylin[1] | Pancreatic β Cells | 1) Suppresses glucagon secretion after eating; 2) Slows gastric emptying; 3) Reduces food intake. | Lowers |
| GLP-1[1] | Intestinal L cells | 1) Enhances glucose-dependent insulin secretion; 2) Suppresses glucagon secretion after eating; 3) Slows gastric emptying; 4) Reduces food intake. (Only works while food is in the gut) | Lowers |
| GIP | Intestinal K cells | 1) Induce insulin secretion 2) Inhibits apoptosis of the pancreatic beta cells and promotes their proliferation 3) Stimulates glucagon secretion and fat accumulation | Lowers |
| Glucagon | Pancreatic α Cells | 1) Enhances release of glucose from glycogen (glycogenolysis); 2) Enhances synthesis of glucose (gluconeogenesis) from amino acids or fats. | Raises |
| Asprosin[8] | White adipose tissue | 1) Enhances release of liver glucose during fasting. | Raises |
| Somatostatin | Pancreatic δ Cells | 1) Suppresses glucagon release from α cells (acts locally); 2) Suppresses release of Insulin, Pituitary tropic hormones, gastrin and secretin. 3) Decreases stomach acid production by preventing the release of other hormones (gastrin and histamine), thus slowing down the digestive process. | Lowers[citation needed] |
| Epinephrine | Adrenal medulla | 1) Enhances release of glucose from glycogen; 2) Enhances release of fatty acids from adipose tissue. | Raises |
| Cortisol | Adrenal cortex | 1) Enhances gluconeogenesis; 2) Antagonizes insulin. | Raises |
| ACTH | Anterior pituitary | 1) Enhances release of cortisol; 2) Enhances release of fatty acids from adipose tissue. | Raises |
| Growth hormone | Anterior pituitary | Antagonizes insulin | Raises |
| Thyroxine | Thyroid | 1) Enhances release of glucose from glycogen; 2) Enhances absorption of sugars from intestine. | Raises |
References
- ^ a b c Aronoff SL, Berkowitz K, Shreiner B, Want L (2004). "Glucose metabolism and regulation: Beyond insulin and glucagon". Diabetes Spectrum. 17 (3): 183–90. doi:10.2337/diaspect.17.3.183.
- ^ BOLIE, VW (September 1961). "Coefficients of normal blood glucose regulation". Journal of Applied Physiology. 16 (5): 783–8. doi:10.1152/jappl.1961.16.5.783. PMID 13870789.
- ^ Matthews, DR; Hosker, JP; Rudenski, AS; Naylor, BA; Treacher, DF; Turner, RC (July 1985). "Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man". Diabetologia. 28 (7): 412–9. doi:10.1007/BF00280883. PMID 3899825. S2CID 24872571.
- ^ Bergman, RN (2020). "Origins and History of the Minimal Model of Glucose Regulation". Frontiers in Endocrinology. 11: 583016. doi:10.3389/fendo.2020.583016. PMC 7917251. PMID 33658981.
- ^ Dietrich, JW; Dasgupta, R; Anoop, S; Jebasingh, F; Kurian, ME; Inbakumari, M; Boehm, BO; Thomas, N (21 October 2022). "SPINA Carb: a simple mathematical model supporting fast in-vivo estimation of insulin sensitivity and beta cell function". Scientific Reports. 12 (1): 17659. Bibcode:2022NatSR..1217659D. doi:10.1038/s41598-022-22531-3. PMC 9587026. PMID 36271244. S2CID 253041870.
- ^ Gandasi, Nikhil R.; Yin, Peng; Omar-Hmeadi, Muhmmad; Laakso, Emilia Ottosson; Vikman, Petter; Barg, Sebastian (2018-02-06). "Glucose-Dependent Granule Docking Limits Insulin Secretion and Is Decreased in Human Type 2 Diabetes". Cell Metabolism. 27 (2): 470–478.e4. doi:10.1016/j.cmet.2017.12.017. ISSN 1550-4131. PMID 29414688.
- ^ Ebey Soman, Scienceray, Regulation of Glucose by Insulin Archived July 16, 2011, at the Wayback Machine, May 4, 2009. Retrieved November 1, 2009.
- ^ Romere C, Duerrschmid C, Bournat J, Constable P, Jain M, Xia F, Saha PK, Del Solar M, Zhu B, York B, Sarkar P, Rendon DA, Gaber MW, LeMaire SA, Coselli JS, Milewicz DM, Sutton VR, Butte NF, Moore DD, Chopra AR (April 2016). "Asprosin, a Fasting-Induced Glucogenic Protein Hormone". Cell. 165 (3): 566–79. doi:10.1016/j.cell.2016.02.063. PMC 4852710. PMID 27087445.
