Alcohol (drug)
 | |||
| |||
| Clinical data | |||
|---|---|---|---|
| Pronunciation | /ˈɛθənɒl/ | ||
| Other names | Absolute alcohol; Alcohol (USP); Cologne spirit; Drinking alcohol; Ethanol (JAN); Ethylic alcohol; EtOH; Ethyl alcohol; Ethyl hydrate; Ethyl hydroxide; Ethylol; Grain alcohol; Hydroxyethane; Methylcarbinol | ||
| Pregnancy category |
| ||
| Dependence liability | Physical: Very High Psychological: Moderate[1] | ||
| Addiction liability | Moderate (10–15%)[2] | ||
| Routes of administration | Common: By mouth Uncommon: Suppository, inhalation, ophthalmic, insufflation, injection[3] | ||
| Drug class | Depressant; Anxiolytic; Analgesic; Euphoriant; Sedative; Emetic; Diuretic; General anesthetic | ||
| ATC code | |||
| Legal status | |||
| Legal status |
| ||
| Pharmacokinetic data | |||
| Bioavailability | 80%+[4][5] | ||
| Protein binding | Weakly or not at all[4][5] | ||
| Metabolism | Liver (90%):[6][8] • Alcohol dehydrogenase • MEOS (CYP2E1) | ||
| Metabolites | Acetaldehyde; Acetic acid; Acetyl-CoA; Carbon dioxide; Ethyl glucuronide; Ethyl sulfate; Water | ||
| Onset of action | Peak concentrations:[6][4] • Range: 30–90 minutes • Mean: 45–60 minutes • Fasting: 30 minutes | ||
| Elimination half-life | Constant-rate elimination at typical concentrations:[7][8][6] • Range: 10–34 mg/dL/hour • Mean (men): 15 mg/dL/hour • Mean (women): 18 mg/dL/hr At very high concentrations (t1/2): 4.0–4.5 hours[5][4] | ||
| Duration of action | 6–16 hours (amount of time that levels are detectable)[9] | ||
| Excretion | • Major: metabolism (into carbon dioxide and water)[4] • Minor: urine, breath, sweat (5–10%)[6][4] | ||
| Identifiers | |||
| |||
| CAS Number | |||
| PubChem CID | |||
| IUPHAR/BPS | |||
| DrugBank | |||
| ChemSpider | |||
| UNII | |||
| KEGG | |||
| ChEBI | |||
| ChEMBL | |||
| PDB ligand | |||
| Chemical and physical data | |||
| Formula | C2H6O | ||
| Molar mass | 46.069 g·mol−1 | ||
| 3D model (JSmol) | |||
| Density | 0.7893 g/cm3 (at 20 °C)[10] | ||
| Melting point | −114.14 ± 0.03 °C (−173.45 ± 0.05 °F) [10] | ||
| Boiling point | 78.24 ± 0.09 °C (172.83 ± 0.16 °F) [10] | ||
| Solubility in water | Miscible mg/mL (20 °C) | ||
| |||
| |||
Alcohol (from Arabic al-kuḥl 'the kohl'),[11] sometimes referred to by the chemical name ethanol, is the second most consumed psychoactive drug globally behind caffeine,[12] and one of the most widely abused drugs in the world.[13] It is a central nervous system (CNS) depressant, decreasing electrical activity of neurons in the brain.[14] The World Health Organization (WHO) classifies alcohol as a toxic, psychoactive, dependence-producing, and carcinogenic substance.[15]
Alcohol is found in fermented beverages such as beer, wine, and distilled spirit[16] – in particular, rectified spirit,[17] and serves various purposes; Certain religions integrate alcohol into their spiritual practices. For example, Roman Catholicism incorporates sacramental wine in religious rites such as the Eucharist, and permits moderate consumption of alcohol in daily life as a means of experiencing joy.[18] Alcohol is also used as a recreational drug, for example by college students, for self-medication, and in warfare. It is also frequently involved in alcohol-related crimes such as drunk driving, public intoxication, and underage drinking.
Short-term effects from moderate consumption include relaxation, decreased social inhibition, and euphoria, while binge drinking may result in cognitive impairment, blackout, and hangover. Excessive alcohol intake causes alcohol poisoning, characterized by unconsciousness or, in severe cases, death. Long-term effects are considered to be a major global public health issue and includes alcoholism, abuse, alcohol withdrawal, fetal alcohol spectrum disorder (FASD), liver disease, hepatitis, cardiovascular disease (e.g., cardiomyopathy), polyneuropathy, alcoholic hallucinosis, long-term impact on the brain (e.g., brain damage, dementia, and Marchiafava–Bignami disease), and cancers.
For roughly two decades, the International Agency for Research on Cancer (IARC) of the WHO has classified alcohol as a Group 1 Carcinogen.[19] Globally, alcohol use was the seventh leading risk factor for both deaths and DALY in 2016.[20] According to WHO's Global status report on alcohol and health 2018, more than 200 health issues are associated with harmful alcohol consumption, ranging from liver diseases, road injuries and violence, to cancers, cardiovascular diseases, suicides, tuberculosis, and HIV/AIDS.[21] Moreover, a 2024 WHO report indicates that these harmful consequences of alcohol use result in approximately 2.6 million deaths annually, accounting for 4.7% of all global deaths.[22]
In 2023, the WHO declared that 'there is no safe amount of alcohol consumption' and that 'the risk to the drinker’s health starts from the first drop of any alcoholic beverage.'[15] This new global health policy aligns with the scientific consensus regarding the risks of alcohol consumption for pregnant women, particularly due to FASDs, as well as for individuals under the legal drinking age. Additionally, this social change also reflects the temperance movement's opposition to alcohol consumption and is supported by national public health agencies, which increasingly recommend abstinence in their alcohol consumption recommendations while noting that any alcohol intake raises risk levels.[23][24][25]
Uses
Medical
Spiritus fortis is a medical term for ethanol solutions with 95% ABV.
When taken by mouth or injected into a vein ethanol is used to treat methanol or ethylene glycol toxicity[26] when fomepizole is not available.[27]
Ethanol, when used to treat or prevent methanol and/or ethylene glycol toxicity, competes with other alcohols for the alcohol dehydrogenase enzyme, lessening metabolism into toxic aldehyde and carboxylic acid derivatives, and reducing the more serious toxic effects of the glycols when crystallized in the kidneys.[28]
Recreational
Drinking culture is the set of traditions and social behaviors that surround the consumption of alcoholic beverages as a recreational drug and social lubricant. Although alcoholic beverages and social attitudes toward drinking vary around the world, nearly every civilization has independently discovered the processes of brewing beer, fermenting wine and distilling spirits.[29]
Common drinking styles include moderate drinking, social drinking, and binge drinking.
Drinking styles

Source: SAMHSA[30]
In today's society, there is a growing awareness of this, reflected in the variety of approaches to alcohol use, each emphasizing responsible choices. Sober curious describes a mindset or approach where someone is consciously choosing to reduce or eliminate alcohol consumption, not drinking and driving, being aware of your surroundings, not pressuring others to drink, and being able to quit anytime. However, they are not necessarily committed to complete sobriety.
Binge drinking
Binge drinking, or heavy episodic drinking, is drinking alcoholic beverages with an intention of becoming intoxicated by heavy consumption of alcohol over a short period of time, but definitions vary considerably.[31] Binge drinking is a style of drinking that is popular in several countries worldwide, and overlaps somewhat with social drinking since it is often done in groups.
Drinking games involve consuming alcohol as part of the gameplay. They can be risky because they can encourage people to drink more than they intended to. Recent studies link binge drinking habits to a decline in quality of life and a shortened lifespan by 3–6 years.[32][33]
Alcohol-based sugar-sweetened beverages, are closely linked to episodic drinking in adolescents.[34] Sugar-infused alcoholic beverages include alcopops, and liqueurs.
Definition
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) defines binge drinking as a pattern of alcohol consumption that brings a person's blood alcohol concentration (BAC) to 0.08 percent or above. This typically occurs when men consume five or more US standard drinks, or women consume four or more drinks, within about two hours. The Substance Abuse and Mental Health Services Administration (SAMHSA) defines binge drinking slightly differently, focusing on the number of drinks consumed on a single occasion. According to SAMHSA, binge drinking is consuming five or more drinks for men, or four or more drinks for women, on the same occasion on at least one day in the past month.[35]
Light, moderate, responsible, and social drinking
Light drinking, moderate drinking, responsible drinking, and social drinking are often used interchangeably, but with slightly different connotations:
- Light drinking - "Alcohol has been found to increase risk for cancer, and for some types of cancer, the risk increases even at low levels of alcohol consumption (less than 1 drink in a day). Caution, therefore, is recommended.", according to the Dietary Guidelines for Americans (DGA).[36] "The Committee recommended that adults limit alcohol intake to no more than 1 drink per day for both women and men for better health" (DGA).[37] "At least 12 drinks in the past year but 3 drinks or fewer per week, on average over the past year.", according to the Centers for Disease Control and Prevention (CDC).[38]
- Moderate drinking - strictly focuses on the amount of alcohol consumed, following alcohol consumption recommendations. This is called "drinking in moderation". The CDC defines "Current moderate drinker – More than 3 drinks but no more than 7 drinks per week for women and more than 3 drinks but no more than 14 drinks per week for men, on average over the past year.".[38]
- According to the WHO nearly half of all alcohol-attributable cancers in the WHO European Region are linked to alcohol consumption, even from "light" or "moderate" drinking – "less than 1.5 litres of wine or less than 3.5 litres of beer or less than 450 millilitres of spirits per week".[15] However, moderate drinking is associated with a further slight increase in cancer risk.[41][42] Also, moderate drinking may disrupt normal brain functioning.[43]
- Responsible drinking - as defined by alcohol industry standards, often emphasizes personal choice and risk management, unlike terms like "social drinking" or "moderate drinking".[44]
- Critics argue that the alcohol industry's definition does not always align with official recommendations for safe drinking limits.[44]
- Social drinking - refers to casual drinking of alcoholic beverages in a social setting (for example bars, nightclubs, or parties) without an intent to become intoxicated. A social drinker is also defined as a person who only drinks alcohol during social events, such as parties, and does not drink while alone (e.g., at home).[45]
- While social drinking often involves moderation, it does not strictly emphasize safety or specific quantities, unlike moderate drinking. Social settings can involve peer pressure to drink more than intended, which can be a risk factor for excessive alcohol consumption. Regularly socializing over drinks can lead to a higher tolerance for alcohol and potentially dependence, especially in groups where drinking is a central activity. Social drinking does not preclude the development of alcohol dependence. High-functioning alcoholism describes individuals who appear to function normally in daily life despite struggling with alcohol dependence.
Heavy drinking

A 2007 study at the University of Texas at Austin monitored the drinking habits of 541 students over two football seasons. It revealed that high-profile game days ranked among the heaviest drinking occasions, similar to New Year's Eve. Male students increased their consumption for all games, while socially active female students drank heavily during away games. Lighter drinkers also showed a higher likelihood of risky behaviors during away games as their intoxication increased. This research highlights specific drinking patterns linked to collegiate sports events.[46]
According to a 2022 study, recreational heavy drinking and intoxication have become increasingly prevalent among Nigerian youth in Benin City. Traditionally, alcohol use was more accepted for men, while youth drinking was often taboo. Today, many young people engage in heavy drinking for pleasure and excitement. Peer networks encourage this behavior through rituals that promote intoxication and provide care for inebriated friends. The findings suggest a need to reconsider cultural prohibitions on youth drinking and advocate for public health interventions promoting low-risk drinking practices.[47]
Definition
Heavy alcohol use is defined differently by various health organizations. The CDC defines "Current heavier drinker" as consuming more than 7 drinks per week for women and more than 14 drinks per week for men. Additionally, "Heavy drinking day (also referred to as episodic heavy drinking" is characterized as having 4 or more drinks on a single occasion for women and 5 or more for men, in the past year.[48] The National Institute on Alcohol Abuse and Alcoholism (NIAAA) provides gender-specific guidelines for heavy drinking. According to NIAAA, men who consume five or more US standard drinks in a single day or 15 or more drinks within a week are considered heavy drinkers. For women, the threshold is lower, with four or more drinks in a day or eight or more drinks per week classified as heavy drinking. In contrast, the Substance Abuse and Mental Health Services Administration (SAMHSA) takes a different approach to defining heavy alcohol use. SAMHSA considers heavy alcohol use to be engaging in binge drinking behaviors on five or more days within a month. This definition focuses more on the frequency of excessive drinking episodes rather than specific drink counts.[35]
Despite this risk, a 2014 report in the National Survey on Drug Use and Health found that only 10% of either "heavy drinkers" or "binge drinkers" defined according to the above criteria also met the criteria for alcohol dependence, while only 1.3% of non-binge drinkers met the criteria. An inference drawn from this study is that evidence-based policy strategies and clinical preventive services may effectively reduce binge drinking without requiring addiction treatment in most cases.[49]
Self-medication

The therapeutic index for ethanol is 10%.[50]
Alcohol can have analgesic (pain-relieving) effects, which is why some people with chronic pain turn to alcohol to self-medicate and try to alleviate their physical discomfort.[51]
People with social anxiety disorder commonly self-medicate with alcohol to overcome their highly set inhibitions.[52] However, self-medicating excessively for prolonged periods of time with alcohol often makes the symptoms of anxiety or depression worse. This is believed to occur as a result of the changes in brain chemistry from long-term use.[53][54][55] A 2023 systematic review highlights the non-addictive use of alcohol for managing developmental issues, personality traits, and psychiatric symptoms, emphasizing the need for informed, harm-controlled approaches to alcohol consumption within a personalized health policy framework.[56]
A 2023 study suggests that people who drink for both recreational enjoyment and therapeutic reasons, like relieving pain and anxiety/depression/stress, have a higher demand for alcohol compared to those who drink solely for recreation or self-medication. This finding raises concerns, as this group may be more likely to develop alcohol use disorder and experience negative consequences related to their drinking.[57] A significant proportion of patients attending mental health services for conditions including anxiety disorders such as panic disorder or social phobia have developed these conditions as a result of recreational alcohol or sedative use.
Self-medication or mental disorders may make people not decline their drinking despite negative consequences. This can create a cycle of dependence that is difficult to break without addressing the underlying mental health issue.
Unscientific

The American Heart Association warn that "We've all seen the headlines about studies associating light or moderate drinking with health benefits and reduced mortality. Some researchers have suggested there are health benefits from wine, especially red wine, and that a glass a day can be good for the heart. But there's more to the story. No research has proved a cause-and-effect link between drinking alcohol and better heart health."[59]
In folk medicine, consuming a nightcap is for the purpose of inducing sleep. However, alcohol is not recommended by many doctors as a sleep aid because it interferes with sleep quality.[60]
"Hair of the dog", short for "hair of the dog that bit you", is a colloquial expression in the English language predominantly used to refer to alcohol that is consumed as a hangover remedy (with the aim of lessening the effects of a hangover). Many other languages have their own phrase to describe the same concept. The idea may have some basis in science in the difference between ethanol and methanol metabolism. Instead of alcohol, rehydration before going to bed or during hangover may relieve dehydration-associated symptoms such as thirst, dizziness, dry mouth, and headache.[61][62][63][64][65][66]
Drinking alcohol may cause subclinical immunosuppression.[67]
Dutch courage

Dutch courage, also known as pot-valiance or liquid courage, refers to courage gained from intoxication with alcohol.
Alcohol use among college students is often used as "liquid courage" in the hookup culture, for them to make a sexual advance in the first place.[68]: 200 However, a recent trend called "dry dating" is gaining popularity to replace "liquid courage", which involves going on dates without consuming alcohol.[69][70][71]
Consuming alcohol prior to visiting female sex workers is a common practice among some men.[72] Sex workers often resort to using drugs and alcohol to cope with stress.[73]
Alcohol when consumed in high doses is considered to be an anaphrodisiac.[74]
Criminal
Albeit not a valid intoxication defense, weakening the inhibitions by drunkenness is occasionally used as a tool to commit planned offenses such as property crimes including theft and robbery, and violent crimes including assault, murder, or rape – which sometimes but not always occurs in alcohol-facilitated sexual assaults where the victim is also drugged.
Warfare

Alcohol has a long association of military use, and has been called "liquid courage" for its role in preparing troops for battle, anaesthetize injured soldiers, and celebrate military victories. It has also served as a coping mechanism for combat stress reactions and a means of decompression from combat to everyday life. However, this reliance on alcohol can have negative consequences for physical and mental health.[75] Military and veteran populations face significant challenges in addressing the co-occurrence of PTSD and alcohol use disorder.[76] Military personnel who show symptoms of PTSD, major depressive disorder, alcohol use disorder, and generalized anxiety disorder show higher levels of suicidal ideation.[77]
Alcohol consumption in the US Military is higher than any other profession, according to CDC data from 2013–2017. The Department of Defense Survey of Health Related Behaviors among Active Duty Military Personnel published that 47% of active duty members engage in binge drinking, with another 20% engaging in heavy drinking in the past 30 days.
Reports from the Russian invasion of Ukraine in 2022 and since suggested that Russian soldiers are drinking significant amount of alcohol (as well as consuming harder drugs), which increases their losses. Some reports suggest that on occasion, alcohol and drugs have been provided to the lower quality troops by their commanders, in order to facilitate their use as expendable cannon fodder.[78][79][80][81]
Food energy

The USDA uses a figure of 6.93 kilocalories (29.0 kJ) per gram of alcohol (5.47 kcal or 22.9 kJ per ml) for calculating food energy.[82] For distilled spirits, a standard serving in the United States is 44 ml (1.5 US fl oz), which at 40% ethanol (80 proof), would be 14 grams and 98 calories.
However, alcoholic drinks are considered empty calorie foods because other than food energy they contribute no essential nutrients. Alcohol increases insulin response to glucose promoting fat storage and hindering carb/fat burning oxidation.[83][84] This excess processing in the liver acetyl CoA can lead to fatty liver disease and eventually alcoholic liver disease. This progression can lead to further complications, alcohol-related liver disease may cause exocrine pancreatic insufficiency, the inability to properly digest food due to a lack or reduction of digestive enzymes made by the pancreas.[85]
The use of alcohol as a staple food source is considered inconvenient due to the fact that it increases the blood alcohol content (BAC). However, alcohol is a significant source of food energy for individuals with alcoholism and those who engage in binge drinking; For example, individuals with drunkorexia, engage in the combination of self-imposed malnutrition and binge drinking to avoid weight gain from alcohol, to save money for purchasing alcohol,[86] and to facilitate alcohol intoxication.[87] Also, in alcoholics who get most of their daily calories from alcohol, a deficiency of thiamine can produce Korsakoff's syndrome, which is associated with serious brain damage.[88]
Spiritual

Christian views on alcohol encompass a range of perspectives regarding the consumption of alcoholic beverages, with significant emphasis on moderation rather than total abstinence. The moderationist position is held by Roman Catholics[18] and Eastern Orthodox,[89] and within Protestantism, it is accepted by Anglicans,[90] Lutherans[91][92] and many Reformed churches.[93][94][95][96] Moderationism is also accepted by Jehovah's Witnesses.[97]
Spiritual use of moderate alcohol consumption is also found in some religions and schools with esoteric influences, including the Hindu tantra sect Aghori, in the Sufi Bektashi Order and Alevi Jem ceremonies,[98] in the Rarámuri religion, in the Japanese religion Shinto,[99] by the new religious movement Thelema, in Vajrayana Buddhism, and in Vodou faith of Haiti.
Contraindication
Pregnancy

In the US, alcohol is subject to the FDA drug labeling Pregnancy Category X (Contraindicated in pregnancy).
Minnesota, North Dakota, Oklahoma, South Dakota, and Wisconsin have laws that allow the state to involuntarily commit pregnant women to treatment if they abuse alcohol during pregnancy.[100]
Risks
Fetal alcohol spectrum disorder

Ethanol is classified as a teratogen[101][102][medical citation needed]—a substance known to cause birth defects; according to the U.S. Centers for Disease Control and Prevention (CDC), alcohol consumption by women who are not using birth control increases the risk of fetal alcohol spectrum disorders (FASDs). This group of conditions encompasses fetal alcohol syndrome, partial fetal alcohol syndrome, alcohol-related neurodevelopmental disorder, static encephalopathy, and alcohol-related birth defects.[103] The CDC currently recommends complete abstinence from alcoholic beverages for women of child-bearing age who are pregnant, trying to become pregnant, or are sexually active and not using birth control.[104]
In South Africa, some populations have rates as high as 9%.[105]
Miscarriage
Miscarriage, also known in medical terms as a spontaneous abortion, is the death and expulsion of an embryo or fetus before it can survive independently.
Alcohol consumption is a risk factor for miscarriage.[106]
Sudden infant death syndrome
Drinking of alcohol by parents is linked to sudden infant death syndrome (SIDS).[107] One study found a positive correlation between the two during New Years celebrations and weekends.[108] Another found that alcohol use disorder was linked to a more than doubling of risk.[109]
Adverse effects

Alcohol has a variety of short-term and long-term adverse effects. Alcohol has both short-term, and long-term effects on the memory, and sleep. It also has reinforcement-related adverse effects, including alcoholism, dependence, and withdrawal; The most severe withdrawal symptoms, associated with physical dependence, can include seizures and delirium tremens, which in rare cases can be fatal. Alcohol use is directly related to considerable morbidity and mortality, for instance due to intoxication and alcohol-related health problems.[110] The World Health Organization advises that there is no safe level of alcohol consumption.[111]
A study in 2015 found that alcohol and tobacco use combined resulted in a significant health burden, costing over a quarter of a billion disability-adjusted life years. Illicit drug use caused tens of millions more disability-adjusted life years.[112]
Drunkorexia is a colloquialism for anorexia or bulimia combined with an alcohol use disorder.[113]
Alcohol is a common cause of substance-induced psychosis or episodes, which may occur through acute intoxication, chronic alcoholism, withdrawal, exacerbation of existing disorders, or acute idiosyncratic reactions.[114] Research has shown that excessive alcohol use causes an 8-fold increased risk of psychotic disorders in men and a 3-fold increased risk of psychotic disorders in women.[115][116] While the vast majority of cases are acute and resolve fairly quickly upon treatment and/or abstinence, they can occasionally become chronic and persistent.[114] Alcoholic psychosis is sometimes misdiagnosed as another mental illness such as schizophrenia.[117]
An inability to process or exhibit emotions in a proper manner has been shown to exist in people who consume excessive amounts of alcohol and those who were exposed to alcohol while fetuses (FAexp).[118] Also, a significant portion (40–60%) of alcoholics experience emotional blindness.[119] Impairments in theory of mind, as well as other social-cognitive deficits, are commonly found in people who have alcohol use disorders, due to the neurotoxic effects of alcohol on the brain, particularly the prefrontal cortex.[120]
Short-term effects

The amount of ethanol in the body is typically quantified by blood alcohol content (BAC); weight of ethanol per unit volume of blood. Small doses of ethanol, in general, are stimulant-like[121] and produce euphoria and relaxation; people experiencing these symptoms tend to become talkative and less inhibited, and may exhibit poor judgement. At higher dosages (BAC > 1 gram/liter), ethanol acts as a central nervous system (CNS) depressant,[121] producing at progressively higher dosages, impaired sensory and motor function, slowed cognition, stupefaction, unconsciousness, and possible death. Ethanol is commonly consumed as a recreational substance, especially while socializing, due to its psychoactive effects.
Central nervous system impairment

Alcohol causes generalized CNS depression, is a positive allosteric GABAA modulator and is associated and related with decreased anxiety, decreased social inhibition, sedation, impairment of cognitive, memory, motor, and sensory function. It slows and impairs cognition and reaction time and the cognitive skills, impairs judgement, interferes with motor function resulting in motor incoordination, numbness, impairs memory formation, and causes sensory impairment.
Binge drinking can cause generalized impairment of neurocognitive function, dizziness, analgesia, amnesia, ataxia (loss of balance, confusion, sedation, slurred speech), general anaesthesia, decreased libido, nausea, vomiting, blackout, spins, stupor, unconsciousness, and hangover.
At very high concentrations, alcohol can cause anterograde amnesia, markedly decreased heart rate, pulmonary aspiration, positional alcohol nystagmus, respiratory depression, shock, coma and death can result due to profound suppression of CNS function alcohol overdose and can finish in consequent dysautonomia.
Gastrointestinal effects

Alcohol can cause nausea and vomiting in sufficiently high amounts (varying by person).
Alcohol stimulates gastric juice production, even when food is not present, and as a result, its consumption stimulates acidic secretions normally intended to digest protein molecules. Consequently, the excess acidity may harm the inner lining of the stomach. The stomach lining is normally protected by a mucosal layer that prevents the stomach from, essentially, digesting itself.[122]
Ingestion of alcohol can initiate systemic pro-inflammatory changes through two intestinal routes: (1) altering intestinal microbiota composition (dysbiosis), which increases lipopolysaccharide (LPS) release, and (2) degrading intestinal mucosal barrier integrity – thus allowing LPS to enter the circulatory system. The major portion of the blood supply to the liver is provided by the portal vein. Therefore, while the liver is continuously fed nutrients from the intestine, it is also exposed to any bacteria and/or bacterial derivatives that breach the intestinal mucosal barrier. Consequently, LPS levels increase in the portal vein, liver and systemic circulation after alcohol intake. Immune cells in the liver respond to LPS with the production of reactive oxygen species, leukotrienes, chemokines and cytokines. These factors promote tissue inflammation and contribute to organ pathology.[123]
Hangover

A hangover is the experience of various unpleasant physiological and psychological effects usually following the consumption of alcohol, such as wine, beer, and liquor. Hangovers can last for several hours or for more than 24 hours. Typical symptoms of a hangover may include headache, drowsiness, concentration problems, dry mouth, dizziness, fatigue, gastrointestinal distress (e.g., nausea, vomiting, diarrhea), absence of hunger, light sensitivity, depression, sweating, hyper-excitability, irritability, and anxiety (often referred to as "hangxiety").[124][125]
Though many possible remedies and folk cures have been suggested, there is no compelling evidence to suggest that any are effective for preventing or treating hangovers.[126][127] Avoiding alcohol or drinking in moderation are the most effective ways to avoid a hangover.[126] The socioeconomic consequences of hangovers include workplace absenteeism, impaired job performance, reduced productivity and poor academic achievement. A hangover may also impair performance during potentially dangerous daily activities such as driving a car or operating heavy machinery.[128]
Holiday heart syndrome

Holiday heart syndrome, also known as alcohol-induced atrial arrhythmias, is a syndrome defined by an irregular heartbeat and palpitations[129] associated with high levels of ethanol consumption.[130][131] Holiday heart syndrome was discovered in 1978 when Philip Ettinger discovered the connection between arrhythmia and alcohol consumption.[132] It received its common name as it is associated with the binge drinking common during the holidays.[133] It is unclear how common this syndrome is. 5-10% of cases of atrial fibrillation may be related to this condition, but it could be as high 63%.[134]
Positional alcohol nystagmus
Positional alcohol nystagmus (PAN) is nystagmus (visible jerkiness in eye movement) produced when the head is placed in a sideways position. PAN occurs when the specific gravity of the membrane space of the semicircular canals in the ear differs from the specific gravity of the fluid in the canals because of the presence of alcohol.[135]
Allergic-like reactions

Ethanol-containing beverages can cause alcohol flush reactions, exacerbations of rhinitis and, more seriously and commonly, bronchoconstriction in patients with a history of asthma, and in some cases, urticarial skin eruptions, and systemic dermatitis. Such reactions can occur within 1–60 minutes of ethanol ingestion, and may be caused by:[138]
- genetic abnormalities in the metabolism of ethanol, which can cause the ethanol metabolite, acetaldehyde, to accumulate in tissues and trigger the release of histamine, or
- true allergy reactions to allergens occurring naturally in, or contaminating, alcoholic beverages (particularly wine and beer), and
- other unknown causes.
Alcohol flush reaction has also been associated with an increased risk of esophageal cancer in those who do drink.[136][139][140]
Long-term effects

According to The Lancet, 'four industries (tobacco, unhealthy food, fossil fuel, and alcohol) are responsible for at least a third of global deaths per year'.[141] In 2024, the World Health Organization published a report including these figures.[142][143]
Due to the long term effects of alcohol abuse, binge drinking is considered to be a major public health issue.[144]
The impact of alcohol on aging is multifaceted. The relationship between alcohol consumption and body weight is the subject of inconclusive studies. Alcoholic lung disease is disease of the lungs caused by excessive alcohol. However, the term 'alcoholic lung disease' is not a generally accepted medical diagnosis.
Alcohol's overall effect on health is uncertain. While some studies suggest moderate consumption might have some benefit, others find any amount increases health risks. This uncertainty is due to conflicting research methods and potential biases, including counting former drinkers as abstainers and the possibility of alcohol industry influence. Because of these issues, experts advise against using alcohol for health reasons. For example, reviews from 2016 found that the "risk of all-cause mortality, and of cancers specifically, rises with increasing levels of consumption, and the level of consumption that minimises health loss is zero".[20] Additionally, in 2023, the World Health Organization (WHO) stated that there is currently no conclusive evidence from studies that the potential benefits of moderate alcohol consumption for cardiovascular disease and type 2 diabetes outweigh the increased cancer risk associated with these drinking levels for individual consumers.[15]
Despite being a widespread issue, social stigma around problematic alcohol use or alcoholism discourages over 80% from seeking help.[145]
Alcoholism
Alcoholism or its medical diagnosis alcohol use disorder refers to alcohol addiction, alcohol dependence, dipsomania, and/or alcohol abuse. It is a major problem and many health problems as well as death can result from excessive alcohol use.[146][110] Alcohol dependence is linked to a lifespan that is reduced by about 12 years relative to the average person.[146] In 2004, it was estimated that 4% of deaths worldwide were attributable to alcohol use.[110] Deaths from alcohol are split about evenly between acute causes (e.g., overdose, accidents) and chronic conditions.[110] The leading chronic alcohol-related condition associated with death is alcoholic liver disease.[110] Alcohol dependence is also associated with cognitive impairment and organic brain damage.[146] Some researchers have found that even one alcoholic drink a day increases an individual's risk of health problems by 0.4%.[147]
Stigma surrounding alcohol use disorder is particularly strong and different from the stigma attached to other mental illnesses not caused by substances.[148] People with this condition are seen less as truly ill, face greater blame and social rejection, and experience higher structural discrimination risks.[149]
Two or more consecutive alcohol-free days a week have been recommended to improve health and break dependence.[150][151]
Dry drunk is an expression coined by the founder of Alcoholics Anonymous[152] that describes an alcoholic who no longer drinks but otherwise maintains the same behavior patterns of an alcoholic.[153]
A high-functioning alcoholic (HFA) is a person who maintains jobs and relationships while exhibiting alcoholism.[154][155][156]
Many Native Americans in the United States have been harmed by, or become addicted to, drinking alcohol.[157]
Brain damage

While many people associate alcohol's effects with intoxication, the long-term impact of alcohol on the brain can be severe. Binge drinking, or heavy episodic drinking, can lead to alcohol-related brain damage that occurs after a relatively short period of time. This brain damage increases the risk of alcohol-related dementia, and abnormalities in mood and cognitive abilities.
Alcohol can cause Wernicke encephalopathy and Korsakoff syndrome which frequently occur simultaneously, known as Wernicke–Korsakoff syndrome.[158] Lesions, or brain abnormalities, are typically located in the diencephalon which result in anterograde and retrograde amnesia, or memory loss.[158]
Dementia
Alcohol-related dementia (ARD) is a form of dementia caused by long-term, excessive consumption of alcohol, resulting in neurological damage and impaired cognitive function.[159]
Marchiafava–Bignami disease

Marchiafava–Bignami disease is a progressive neurological disease of alcohol use disorder, characterized by corpus callosum demyelination and necrosis and subsequent atrophy. The disease was first described in 1903 by the Italian pathologists Amico Bignami and Ettore Marchiafava in an Italian Chianti drinker.[160][161]
Symptoms can include, but are not limited to lack of consciousness, aggression, seizures, depression, hemiparesis, ataxia, apraxia, coma, etc.[162] There will also be lesions in the corpus callosum.[citation needed]
Liver damage

Consuming more than 30 grams of pure alcohol per day over an extended period can significantly increase the risk of developing alcoholic liver disease.[163] During the metabolism of alcohol via the respective dehydrogenases, nicotinamide adenine dinucleotide (NAD) is converted into reduced NAD. Normally, NAD is used to metabolize fats in the liver, and as such alcohol competes with these fats for the use of NAD. Prolonged exposure to alcohol means that fats accumulate in the liver, leading to the term 'fatty liver'. Continued consumption (such as in alcohol use disorder) then leads to cell death in the hepatocytes as the fat stores reduce the function of the cell to the point of death. These cells are then replaced with scar tissue, leading to the condition called cirrhosis.
Cancer

Alcoholic beverages have been classified as carcinogenic by leading health organizations for more than two decades, including the WHO's IARC (Group 1 carcinogens)[19] and the U.S. NTP,[164] raising concerns about the potential cancer risk associated with alcohol consumption.
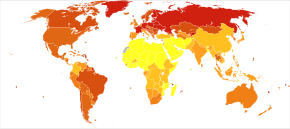
In 2023 the WHO highlighted a statistic: nearly half of all alcohol-attributable cancers in the WHO European Region are linked to alcohol consumption, even from "light" or "moderate" drinking – "less than 1.5 litres of wine or less than 3.5 litres of beer or less than 450 millilitres of spirits per week".[15] This new information suggests that these consumption levels should now be considered high-risk. Many countries exceed these levels by a significant margin. Echoing the WHO's view, a growing number of national public health agencies are prioritizing complete abstinence (teetotalism) and stricter drinking guidelines in their alcohol consumption recommendations.
Alcohol is also a major cause for head and neck cancer, especially laryngeal cancer.
This risk is even higher when alcohol is used together with tobacco.[42][165]
Qualitative analysis reveals that the alcohol industry likely misinforms the public about the alcohol-cancer link, similar to the tobacco industry. The alcohol industry influences alcohol policy and health messages, including those for schoolchildren.[166]
Cardiovascular disease
Excessive daily alcohol consumption and binge drinking can cause a higher risk of stroke, coronary artery disease, heart failure, fatal hypertensive disease, and fatal aortic aneurysm.[167]
A 2010 study reviewed research on alcohol and heart disease. They found that moderate drinking did not seem to worsen things for people who already had heart problems. But importantly, the researchers did not say that people who do not drink should start in order to improve their heart health.[168] Thus, the safety and potential positive effect of light drinking on the cardiovascular system has not yet been proven. Still alcohol is a major health risk, and even if moderate drinking lowers the risk of some cardiovascular diseases it might increase the risk of others. Therefore starting to drink alcohol in the hope of any benefit is not recommended.[167][169]
The World Heart Federation (2022) recommends against any alcohol intake for optimal heart health.[170][171]
It has also been pointed out that the studies suggesting a positive link between red wine consumption and heart health had flawed methodology in the form of comparing two sets of people which were not actually appropriately paired.[171]
Cardiomyopathy

Alcoholic cardiomyopathy (ACM) is a disease in which the long-term consumption of alcohol leads to heart failure.[172] ACM is a type of dilated cardiomyopathy. The heart is unable to pump blood efficiently, leading to heart failure. It can affect other parts of the body if the heart failure is severe. It is most common in males between the ages of 35 and 50.
Hearing loss
Alcohol, classified as an ototoxin (ear toxin),[173] can contribute to hearing loss sometimes referred to as "cocktail deafness" after exposure to loud noises in drinking environments.[174][175]
Children with fetal alcohol spectrum disorder (FASD) are at an increased risk of having hearing difficulties.
Withdrawal syndrome

Discontinuation of alcohol after extended heavy use and associated tolerance development (resulting in dependence) can result in withdrawal. Alcohol withdrawal can cause confusion, paranoia, anxiety, insomnia, agitation, tremors, fever, nausea, vomiting, autonomic dysfunction, seizures, and hallucinations. In severe cases, death can result.
Delirium tremens is a condition that requires people with a long history of heavy drinking to undertake an alcohol detoxification regimen.
Alcohol is one of the more dangerous drugs to withdraw from.[177] Drugs which help to re-stabilize the glutamate system such as N-acetylcysteine have been proposed for the treatment of addiction to cocaine, nicotine, and alcohol.[178]
Cohort studies have demonstrated that the combination of anticonvulsants and benzodiazepines is more effective than other treatments in reducing alcohol withdrawal scores and shortening the duration of intensive care unit stays.[179]
Nitrous oxide has been shown to be an effective and safe treatment for alcohol withdrawal.[180] The gas therapy reduces the use of highly addictive sedative medications (like benzodiazepines and barbiturates).
Cortisol
Research has looked into the effects of alcohol on the amount of cortisol that is produced in the human body. Continuous consumption of alcohol over an extended period of time has been shown to raise cortisol levels in the body. Cortisol is released during periods of high stress, and can result in the temporary shut down of other physical processes, causing physical damage to the body.
Gout

There is a strong association between gout the consumption of alcohol, and sugar-sweetened beverages,[181] with wine presenting somewhat less of a risk than beer or spirits.[182][183]
Ketoacidosis
Alcoholic ketoacidosis (AKA) is a specific group of symptoms and metabolic state related to alcohol use.[184] Symptoms often include abdominal pain, vomiting, agitation, a fast respiratory rate, and a specific "fruity" smell.[185] Consciousness is generally normal.[186] Complications may include sudden death.[186]
Mental disorders
Alcohol misuse often coincides with mental health conditions. Many individuals struggling with psychiatric disorders also experience problematic drinking behaviors.[187] For example, alcohol may play a role in depression, with up to 10% of male depression cases in some European countries linked to alcohol use.[188]
Psychiatric genetics research continues to explore the complex interplay between alcohol use, genetic factors, and mental health outcomes; A 2024 study found that excessive drinking and alcohol-related DNA methylation may directly contribute to the causes of mental disorders, possibly through the altered expression of affected genes.[189]
Austrian syndrome

Austrian syndrome, also known as Osler's triad, is a medical condition that was named after Robert Austrian in 1957. The presentation of the condition consists of pneumonia, endocarditis, and meningitis, all caused by Streptococcus pneumoniae. It is associated with alcoholism due to hyposplenism (reduced splenic functioning) and can be seen in males between the ages of 40 and 60 years old.[190] Robert Austrian was not the first one to describe the condition, but Richard Heschl (around 1860s) or William Osler were not able to link the signs to the bacteria because microbiology was not yet developed.
The leading cause of Osler's triad (Austrian syndrome) is Streptococcus pneumoniae, which is usually associated with heavy alcohol use.
Polyneuropathy
Alcoholic polyneuropathy is a neurological disorder in which peripheral nerves throughout the body malfunction simultaneously. It is defined by axonal degeneration in neurons of both the sensory and motor systems and initially occurs at the distal ends of the longest axons in the body. This nerve damage causes an individual to experience pain and motor weakness, first in the feet and hands and then progressing centrally. Alcoholic polyneuropathy is caused primarily by chronic alcoholism; however, vitamin deficiencies are also known to contribute to its development.
Specific population
Women
Breast cancer
Drinking alcohol increases the risk for breast cancer.[191] For women in Europe, breast cancer represents the most significant alcohol-related cancer burden.[192]
Breastfeeding difficulties
Moderate alcohol consumption by breastfeeding mothers can significantly affect infants and cause breastfeeding difficulties. Even one or two drinks, including beer, may reduce milk intake by 20 to 23%, leading to increased agitation and poor sleep patterns. Regular heavy drinking (more than two drinks daily) can shorten breastfeeding duration and cause issues in infants, such as excessive sedation, fluid retention, and hormonal imbalances. Additionally, higher alcohol consumption may negatively impact children's academic achievement.[193]
Neonatal withdrawal
Babies exposed to alcohol, benzodiazepines, barbiturates, and some antidepressants (SSRIs) during pregnancy may experience neonatal withdrawal.[194]
The onset of clinical presentation typically appears within 48 to 72 hours of birth but may take up to 8 days.[195][196]
Other effects

Excessive alcohol intake has been shown to cause immunodeficiency, compromising the body's ability to fight infections and diseases, as evidenced by research on people who regularly consume large amounts of alcohol.[197][198]
Alcohol is associated with instances of sudden death. Sudden arrhythmic death syndrome in alcohol misuse is a significant cause of death among heavy drinkers, characterized by older age and severe liver damage, highlighting the need for family screening for heritable channelopathies.[199] Also, sudden unexpected death in epilepsy is associated with a twofold higher risk in individuals with a history of substance abuse or alcohol dependence.[200]
Alcohol consumption is associated with lower sperm concentration, percentage of normal morphology, and semen volume, but not sperm motility.[201]
Alcohol consumption may increase the risk of sleep disorders, including insomnia,[202] restless legs syndrome,[203] and sleep apnea.[204]
Frequent drinking of alcoholic beverages is a major contributing factor in cases of hypertriglyceridemia.[205]
Alcoholism is the single most common cause of chronic pancreatitis.[206][207][208][209][210]
Excess alcohol use is frequently associated with porphyria cutanea tarda (PTC).[211]
Alcohol consumption is a risk factor for Dupuytren's contracture.[212][213]
The majority of those with aspirin-exacerbated respiratory disease experience respiratory reactions to alcohol.[214]
Social issues


Alcohol-related crimes
Alcohol use is stereotypically associated with crime,[217] both violent and non-violent.[146] Some crimes are uniquely tied to alcohol, such as public intoxication or underage drinking, while others are simply more likely to occur together with alcohol consumption. Crime perpetrators are much more likely to be intoxicated than crime victims. Many alcohol laws have been passed to criminalize various alcohol-related activities.[217][218] Underage drinking and drunk driving are the most prevalent alcohol-specific offenses in the United States[217] and a major problem in many countries worldwide.[219][220][221] About one-third of arrests in the United States involve alcohol misuse,[146] and arrests for alcohol-related crimes constitute a high proportion of all arrests made by police in the U.S. and elsewhere.[222] In general, programs aimed at reducing society's consumption of alcohol, including education in schools, are seen as an effective long-term solution. Strategies aiming to reduce alcohol consumption among adult offenders have various estimates of effectiveness.[223] Policing alcohol-related street disorder and enforcing compliance checks of alcohol-dispensing businesses has proven successful in reducing public perception of and fear of criminal activities.[217]
In the early 2000s, the monetary cost of alcohol-related crime in the United States alone has been estimated at over $205 billion, twice the economic cost of all other drug-related crimes.[224] In a similar period in the United Kingdom, the cost of crime and its antisocial effects was estimated at £7.3 billion.[223] Another estimate for the UK for yearly cost of alcohol-related crime suggested double that estimate, at between £8 and 13 billion.[225] Risky patterns of drinking are particularly problematic in and around Russia, Mexico and some parts of Africa.[226] Alcohol is more commonly associated with both violent and non-violent crime than are drugs like marijuana.[146]
Passive drinking, like passive smoking, refers to the damage done to others as a result of drinking alcoholic beverages. These include the unborn fetus and children of parents who drink excessively, drunk drivers, accidents, domestic violence and alcohol-related sexual assaults[227]
Public-order crimes
Public-order crimes caused by drinking include drunk driving, domestic violence, and alcohol-related sexual assaults.
Automobile accidents

A 2002 study found 41% of people fatally injured in traffic accidents were in alcohol-related crashes.[228] Misuse of alcohol is associated with more than 40% of deaths that occur in automobile accidents every year.[146] The risk of a fatal car accident increases exponentially with the level of alcohol in the driver's blood.[229]
Most countries have passed laws prohibiting driving a motor vehicle while impaired by alcohol. In the U.S., these crimes are generally referred to as driving under the influence (DUI), although there are many naming variations among jurisdictions, such as driving while intoxicated (DWI).[230] With alcohol consumption, a drunk driver's level of intoxication is typically determined by a measurement of blood alcohol content or BAC; but this can also be expressed as a breath test measurement, often referred to as a BrAC. A BAC or BrAC measurement in excess of the specific threshold level, such as 0.08% in the U.S.,[231] defines the criminal offense with no need to prove impairment.[232] In some jurisdictions, there is an aggravated category of the offense at a higher BAC level, such as 0.12%, 0.15% or 0.25%. In many jurisdictions, police officers can conduct field tests of suspects to look for signs of intoxication.
Negligence

Negligence in alcohol consumption can have a ripple effect on environmentally responsible behavior. Examples:
- Consuming alcoholic beverages, which increases urine production and reduces social inhibitions, can lead to public urination. Public urination is illegal in most areas.
- Improper disposal of alcohol bottles is a common problem. Many are not recycled or left behind in public spaces. Discarded alcoholic beverage containers, especially broken glass shards that are difficult to remove, does not only create an eyesore but may also cause flat tires for cyclists, injure wildlife or kids.
- Alcohol consumption can contribute to nighttime noise pollution, especially through loud music played by intoxicated individuals. This disrupts sleep and relaxation for nearby residents, impacting health and productivity. Municipal noise ordinances often establish quiet hours and penalties for violations.
- People under the influence may forget to extinguish outdoor fireplaces, which may create a fire hazard since unchecked fires can escalate into wildfires.
- Drunk cyclists can only be charged if they ride dangerously, cause a crash, or behave disruptively.[233] However, cycling under the influence increases the risk of severe injury, hospital resource use, and even death, according to a study highlighting the importance of safe cycling practices.[234]
Public drunkenness

Public drunkenness or intoxication is a common problem in many jurisdictions. Public intoxication laws vary widely by jurisdiction, but include public nuisance laws, open-container laws, and prohibitions on drinking alcohol in public or certain areas. The offenders are often lower class individuals and this crime has a very high recidivism rate, with numerous instances of repeated instances of the arrest, jail, release without treatment cycle. The high number of arrests for public drunkenness often reflects rearrests of the same offenders.[222]
Sexual assaults
Rape is any sexual activity that occurs without the freely given consent of one of the parties involved. This includes alcohol-facilitated sexual assault which is considered rape in most if not all jurisdictions,[235] or non-consensual condom removal which is criminalized in some countries (see the map below).
A 2008 study found that rapists typically consumed relatively high amounts of alcohol and infrequently used condoms during assaults, which was linked to a significant increase in STI transmission.[236] This also increase the risk of pregnancy from rape for female victims. Some people turn to drugs or alcohol to cope with emotional trauma after a rape; use of these during pregnancy can harm the fetus.[237]
Alcohol-facilitated sexual assault

One of the most common date rape drugs is alcohol,[239][240][241] administered either surreptitiously[242] or consumed voluntarily,[239] rendering the victim unable to make informed decisions or give consent. The perpetrator then facilitates sexual assault or rape, a crime known as alcohol- or drug-facilitated sexual assault (DFSA).[243][235][244] However, sex with an unconscious victim is considered rape in most if not all jurisdictions, and some assailants have committed "rapes of convenience" whereby they have assaulted a victim after he or she had become unconscious from drinking too much.[245] The risk of individuals either experiencing or perpetrating sexual violence and risky sexual behavior increases with alcohol abuse,[246] and by the consumption of caffeinated alcoholic drinks.[247][248]
Non-consensual condom removal

Non-consensual condom removal, or "stealthing",[249] is the practice of a person removing a condom during sexual intercourse without consent, when their sex partner has only consented to condom-protected sex.[250][251] Purposefully damaging a condom before or during intercourse may also be referred to as stealthing,[252] regardless of who damaged the condom.
Consuming alcohol can be risky in sexual situations. It can impair judgment and make it difficult for both people to give or receive informed sexual consent. However, a history of sexual aggression and alcohol intoxication are factors associated with an increased risk of men employing non-consensual condom removal and engaging in sexually aggressive behavior with female partners.[253][254]
Wartime sexual violence
The use of alcohol is a documented factor in wartime sexual violence.
For example, rape during the liberation of Serbia was committed by Soviet Red Army soldiers against women during their advance to Berlin in late 1944 and early 1945 during World War II. Serbian journalist Vuk Perišić said about the rapes: "The rapes were extremely brutal, under the influence of alcohol and usually by a group of soldiers. The Soviet soldiers did not pay attention to the fact that Serbia was their ally, and there is no doubt that the Soviet high command tacitly approved the rape."[255]
While there was not a codified international law specifically prohibiting rape during World War II, customary international law principles already existed that condemned violence against civilians. These principles formed the basis for the development of more explicit laws after the war,[256] including the Nuremberg Principles established in 1950.
Violent crime

The World Health Organization has noted that out of social problems created by the harmful use of alcohol, "crime and violence related to alcohol consumption" are likely the most significant issue.[226] In the United States, 15% of robberies, 63% of intimate partner violence incidents, 37% of sexual assaults, 45–46% of physical assaults and 40–45% of homicides (murders) involved use of alcohol.[258][224] A 1983 study for the United States found that 54% of violent crime perpetrators, arrested in that country, had been consuming alcohol before their offenses.[222] In 2002, it was estimated that 1 million violent crimes in the U.S. were related to alcohol use.[146] More than 43% of violent encounters with police involve alcohol.[146] Alcohol is implicated in more than two-thirds of cases of intimate partner violence.[146] Studies also suggest there may be links between alcohol abuse and child abuse.[217] In the United Kingdom, in 2015/2016, 39% of those involved in violent crimes were under alcohol influence.[259] A significant portion, 40%, of homicide victims tested positive for alcohol in the US.[260] International studies are similar, with an estimate that 63% of violent crimes worldwide involves the use of alcohol.[224]
The relation between alcohol and violence is not yet fully understood, as its impact on different individuals varies.[citation needed] Studies and theories of alcohol abuse suggest, among others, that use of alcohol likely reduces the offender's perception and awareness of consequences of their actions.[241][217][222][261] Heavy drinking is associated with vulnerability to injury, marital discord, and domestic violence.[146] Moderate drinkers are more frequently engaged in intimate violence than are light drinkers and abstainers, however generally it is heavy and/or binge drinkers who are involved in the most chronic and serious forms of aggression. Research found that factors that increase the likelihood of alcohol-related violence include difficult temperament, hyperactivity, hostile beliefs, history of family violence, poor school performance, delinquent peers, criminogenic beliefs about alcohol's effects, impulsivity, and antisocial personality disorder. The odds, frequency, and severity of physical attacks are all positively correlated with alcohol use. In turn, violence decreases after behavioral marital alcoholism treatment.[217]
Methanol laced alcohol

Outbreaks of methanol poisoning have occurred when methanol is used to lace moonshine (bootleg liquor).[262] This is commonly done to bulk up the original product to gain profit.
India has a thriving moonshine industry, and methanol-tainted batches have killed over 2,000 people in the last 3 decades.
Methanol is a toxic alcohol. If as little as 10 mL (about 1/4th of a US standard shot size (44 mL)) of pure methanol is ingested, for example, it can break down into formic acid, which can cause permanent blindness by destruction of the optic nerve, and 30 mL is potentially fatal,[263] although the median lethal dose is typically 100 mL (3.4 fl oz) (i.e. 1–2 mL/kg body weight of pure methanol[264]). Reference dose for methanol is 2.0 mg/kg/day.[265] Toxic effects take hours to start, and effective antidotes can often prevent permanent damage.[263]
Distinguishing between safe, drinkable ethanol and toxic methanol is extremely challenging through sight, or touch alone, especially when drunk, which dramatically impairs sensory perception and judgment. It is crucial to emphasize that suspected methanol should never be tasted due to its high toxicity; even small amounts can lead to severe health consequences or death. Also, a flame color testing may not be reliable. Both ethanol and methanol are primary alcohols, meaning they have a hydroxyl group (-OH) attached to a terminal carbon atom in their molecular structure. This structural similarity contributes to their comparable physical characteristics and underscores the difficulty in differentiating them through casual observation or sensory perception alone. A proper chemical analysis should be performed by a qualified chemist to accurately distinguish between the two substances.
Alternative routes of administration
Alternative methods of alcohol administration like alcohol enema, alcohol inhalation, vodka eyeballing, or using alcohol powder (which can be added to water to make an alcoholic beverage, or inhaled with a nebulizer), all carry significant health risks.
Binge drinking

Binge drinking is a style of drinking that is popular in several countries worldwide, and overlaps somewhat with social drinking since it is often done in groups. The degree of intoxication however, varies between and within various cultures that engage in this practice. A binge on alcohol can occur over hours, last up to several days, or in the event of extended abuse, even weeks. Due to the long term effects of alcohol abuse, binge drinking is considered to be a major public health issue.[144]
Binge drinking is more common in males, during adolescence and young adulthood. Heavy regular binge drinking is associated with adverse effects on neurologic, cardiac, gastrointestinal, hematologic, immune, and musculoskeletal organ systems as well as increasing the risk of alcohol induced psychiatric disorders.[266][267] A US-based review of the literature found that up to one-third of adolescents binge-drink, with 6% reaching the threshold of having an alcohol-related substance use disorder.[268] Approximately one in 25 women binge-drinks during pregnancy, which can lead to fetal alcohol syndrome and fetal alcohol spectrum disorders.[269] Binge drinking during adolescence is associated with traffic accidents and other types of accidents, violent behavior as well as suicide. The more often a child or adolescent binge drinks and the younger they are the more likely that they will develop an alcohol use disorder including alcoholism. A large number of adolescents who binge-drink also consume other psychotropic substances.[270]
Emotional issues
In emotional self-regulation, some people turn to drugs such as alcohol. Drug use, an example of response modulation, can be used to alter emotion-associated physiological responses. For example, alcohol can produce sedative and anxiolytic effects.[271] A 2013 study found that immature defense mechanisms are linked to placing a higher value on junk food, alcohol, and television.[272]
There is a two-way street between loneliness and drinking. People who drink more than once a week tend to feel lonelier, according to a study on Japanese workers during the COVID-19 pandemic.[273] On the other hand, feelings of loneliness can also lead people to drink more, as shown in a separate study.[274] Loneliness is a major risk factor for depression and alcoholism.[275]
Hurtful communication
Alcohol may cause hurtful communication.
Drunk dialing
Drunk dialing refers to an intoxicated person making phone calls that they would not likely make if sober, often a lonely individual calling former or current love interests.
A 2021 study, that examined the relationship between drunk texting and emotional dysregulation, found a positive correlation. The findings suggest that interventions targeting emotional regulation skills may be beneficial.[276]
In vino veritas
In vino veritas is a Latin phrase that means 'in wine, there is truth', suggesting a person under the influence of alcohol is more likely to speak their hidden thoughts and desires.
Parental supervision of alcohol consumption for minors
Some parents are willing to provide alcohol for their children if they drink it in a controlled environment. Furnishing alcohol to one's own children is permitted in 31 states, while it's illegal to do so for other people's children in all fifty states.[277] However, despite research indicating negative consequences, many parents mistakenly believe that providing alcohol to their underage children will protect them from drinking-related harm. This misconception persists even though studies have shown a connection between parental alcohol supply and unfavorable outcomes related to alcohol consumption among minors.[278] Parental provision of alcohol during childhood may raise the risk of risky drinking in adolescence. However, methodological limitations hinder causal conclusions. To clarify this relationship, more robust longitudinal studies are needed that differentiate between sips and full drinks, accurately measure confounding factors, and apply multivariable adjustments.[279]
Parental attitudes that are less restrictive regarding children's alcohol consumption are linked to an earlier onset of alcohol use, increased frequency of use, and higher instances of drunkenness among children. Additionally, when children perceive their parents as having more lenient attitudes towards alcohol, they are more likely to engage in drinking themselves.[280] Adolescents permitted to drink by their parents were more likely to quickly move from their first drink to binge drinking (5 or more drinks at once) and heavy drinking (3 or more times in the past year). These findings contradict the belief that parental approval of underage drinking protects against alcohol misuse, highlighting the risks associated with adolescent heavy drinking.[281]
Parents may face significant legal consequences in various countries and jurisdictions if they knowingly allow their children to drink alcohol without supervision. This liability arises from a perceived failure to protect the child from the risks associated with alcohol consumption, which could lead to investigations by child protective services.
Risky sexual behavior
Some studies have made a connection between hookup culture and substance use.[282] Most students said that their hookups occurred after drinking alcohol.[282][283][284] Frietas stated that in her study, the relationships between drinking and the party scene and between alcohol and hookup culture were "impossible to miss".[285]: 41
Studies suggest that the degree of alcoholic intoxication in young people directly correlates with the level of risky behavior,[286] such as engaging in multiple sex partners.[287]
In 2018, the first study of its kind, found that alcohol and caffeinated energy drinks is linked with casual, risky sex among college-age adults.[248]
Sexually transmitted infections and unintended pregnancy

Alcohol intoxication is associated with an increased risk that people will become involved in risky sexual behaviors, such as unprotected sex.[288] Both men,[289] and women,[290] reported higher intentions to avoid using a condom when they were intoxicated by alcohol.
Coitus interruptus, also known as withdrawal, pulling out or the pull-out method, is a method of birth control during penetrative sexual intercourse, whereby the penis is withdrawn from a vagina or anus prior to ejaculation so that the ejaculate (semen) may be directed away in an effort to avoid insemination.[291][292] Coitus interruptus carries a risk of sexually transmitted infections (STIs) and unintended pregnancy. This risk is especially high during alcohol intoxication because lowered sexual inhibition can make it difficult to withdraw in time.
Women with unintended pregnancies are more likely to smoke tobacco,[293] drink alcohol during pregnancy,[294][295] and binge drink during pregnancy,[293] which results in poorer health outcomes.[294] (See also: fetal alcohol spectrum disorder)
The relationship between drinking alcohol and how HIV develops and progresses in people has been the subject of prior research investigations.[296][297][298][299] To date, HIV has been recognized as an alcohol-attributable STI in the World Health Organization’s (WHO) most recent comparative risk assessment or related exercises.[21][299]
A systematic review of studies examining alcohol consumption and HIV/AIDS found a strong association between alcohol use, increased HIV incidence, and the worsening of HIV disease progression.[300] Alcohol consumption was linked to risky sexual behaviors, including unprotected sex and having multiple sexual partners, which increase the risk of HIV transmission. Additionally, alcohol negatively impacts the immune system and can reduce adherence to antiretroviral therapy in HIV-positive individuals, potentially accelerating disease progression. While these associations were consistently observed across studies, the review concluded that the available evidence was insufficient to definitively establish a causal link between alcohol use and HIV acquisition or transmission.[300]
A more recent review further supports the strong association between alcohol use, HIV incidence, and HIV/AIDS progression. This review found that alcohol consumption increased the likelihood of risky behaviors, such as unprotected sex, and concluded there is sufficient evidence to suggest a causal relationship between alcohol use and HIV incidence.[299]
Societal damage

Alcohol causes a plethora of detrimental effects in society.[146] A 2023 systematic review estimated the societal costs of alcohol use to be around 2.6% of the GDP.[301] Many emergency room visits involve alcohol use.[146] Alcohol availability and consumption rates and alcohol rates are positively associated with nuisance, loitering, panhandling, and disorderly conduct in public space.[217]
A 2011 study challenged the perception of heroin as the more dangerous substance. The research suggests, when considering the wider social, physical, and financial costs, alcohol may be more harmful.[302]
Individuals who engage with or share alcohol-related content on social networking services tend to exhibit higher levels of alcohol use and related issues.[303] Overwork is linked to an increased risk of unhealthy alcohol consumption.[304] Also, unemployment can heighten the risk of alcohol consumption and smoking.[305] As many as 15% of employees show problematic alcohol-related behaviors in the workplace, such as drinking before going to work or even drinking on the job.[146]
College
Many students attending colleges, universities, and other higher education institutions consume alcoholic beverages. The laws and social culture around this practice vary by country and institution type, and within an institution, some students may drink heavily whereas others may not drink at all. In the United States, drinking tends to be particularly associated with fraternities.
Alcohol abuse among college students refers to unhealthy alcohol drinking behaviors by college and university students. While the legal drinking age varies by country, the high number of underage students that consume alcohol has presented many problems and consequences for universities. The causes of alcohol abuse tend to be peer pressure, fraternity or sorority involvement, and stress. College students who abuse alcohol can suffer from health concerns, poor academic performance or legal consequences. Prevention and treatment include campus counseling, stronger enforcement of underage drinking or changing the campus culture.
Recent research indicates that the abundance of alcohol retailers and the availability of inexpensive alcoholic beverages are linked to heavy alcohol consumption among college students.[306]
Occupational risks

A bargirl is a woman who is paid to entertain patrons in a bar or nightclub. A bar fine is a payment made by a customer to the operators of a bar or nightclub in East and Southeast Asia, allowing her to leave work early, typically to accompany a customer outside for sexual services.[307] Female sex workers in low- and middle-income countries have high rates of harmful alcohol use, which is associated with increased risk of risky sexual behavior.[73] Screening carried out in the 1990s in Malawi, an African country, indicated that about 80 per cent of bargirls carried the HIV virus. Research carried out at the time indicated that economic necessity was a major consideration in engaging and persisting in sex work.[308]
A 2022 study found that bartenders experience high levels of hazardous alcohol and drug use, particularly among those working over 40 hours a week, with males and individuals aged 26–40 exhibiting the most problematic consumption, underscoring the need for targeted preventative interventions and further investigation into the underlying risk factors.[309]
Poverty

Alcohol consumption can contribute to secondary poverty (where people fall back into poverty after escaping it). The Bureau of Labor Statistics found that "the average American consumer dedicates 1 percent of all their spending to alcohol".[310]
Homelessness and poverty are interrelated.[311] Conditions such as alcoholism and mental illness are often associated with homelessness.[312] For people in Russia, especially the youth, alcohol, and substance use is a major cause and reason for becoming and continuing to be homeless.[313] Also, street children from areas with limited resources have reported a high lifetime prevalence of substance use. The most commonly used substances are inhalants, followed by tobacco, alcohol, and marijuana.[314]
Unsustainable tourism
Some popular tourist destinations, are cracking down on the impacts of tourism from excessive drinking. In an effort to promote a more sustainable tourism industry, these locations are implementing new regulations to curb binge drinking. This includes Llucmajor, Palma, Calvia (Magaluf) in Majorca and Sant Antoni in Ibiza, where late-night sales of alcohol will be banned. This comes after years of issues with rowdy tourists and the negative impacts it has on local residents.[315]
Suicide
Most people are under the influence of sedative-hypnotic drugs (such as alcohol or benzodiazepines) when they die by suicide,[316] with alcoholism present in between 15% and 61% of cases.[317] Countries that have higher rates of alcohol use and a greater density of bars generally also have higher rates of suicide.[318] About 2.2–3.4% of those who have been treated for alcoholism at some point in their life die by suicide.[318] Alcoholics who attempt suicide are usually male, older, and have tried to take their own lives in the past.[317] In adolescents who misuse alcohol, neurological and psychological dysfunctions may contribute to the increased risk of suicide.[319]
Interactions
Disorders
COVID-19
A 2023 study suggests a link between alcohol consumption and worse COVID-19 outcomes. Researchers analyzed data from over 1.6 million people and found that any level of alcohol consumption increased the risk of severe illness, intensive care unit admission, and needing ventilation compared to non-drinkers. Even a history of drinking was associated with a higher risk of severe COVID-19. These findings suggest that avoiding alcohol altogether might be beneficial during the pandemic.[320]
Diabetes
See the insulin section.
Hepatitis
Alcohol consumption can be especially dangerous for those with pre-existing liver damage from hepatitis B or C. Even relatively low amounts of alcohol can be life-threatening in these cases,[321] so a strict adherence to abstinence is highly recommended.[322]
Histamine intolerance
Alcohol may release histamine in individuals with histamine intolerance.[323]
Mental disorders
Mental disorders can be a significant risk factor for alcohol abuse.
Alcohol abuse, alcohol dependence, and alcoholism are comorbid with anxiety disorders.[324][325] With dual diagnosis, the initial symptoms of mental illness tend to appear before those of substance abuse.[326] Individuals with common mental health conditions, such as depression, anxiety, or phobias, are twice as likely to also report having an alcohol use disorder, compared to those without these mental health challenges.[327] Alcohol is a major risk factor for self-harm.[328] Individuals with anxiety disorders who self-medicate with drugs or alcohol may also have an increased likelihood of suicidal ideation.[329]
Peptic ulcer disease
In patients who have a peptic ulcer disease (PUD), the mucosal layer is broken down by ethanol. PUD is commonly associated with the bacteria Helicobacter pylori, which secretes a toxin that weakens the mucosal wall, allowing acid and protein enzymes to penetrate the weakened barrier. Because alcohol stimulates the stomach to secrete acid, a person with PUD should avoid drinking alcohol on an empty stomach. Drinking alcohol causes more acid release, which further damages the already-weakened stomach wall.[330] Complications of this disease could include a burning pain in the abdomen, bloating and in severe cases, the presence of dark black stools indicate internal bleeding.[122] A person who drinks alcohol regularly is strongly advised to reduce their intake to prevent PUD aggravation.[122]
Dosage forms
Alcohol induced dose dumping (AIDD)
Alcohol-induced dose dumping (AIDD) is by definition an unintended rapid release of large amounts of a given drug, when administered through a modified-release dosage while co-ingesting ethanol.[331] This is considered a pharmaceutical disadvantage due to the high risk of causing drug-induced toxicity by increasing the absorption and serum concentration above the therapeutic window of the drug. The best way to prevent this interaction is by avoiding the co-ingestion of both substances or using specific controlled-release formulations that are resistant to AIDD.
Drugs
Alcohol can intensify the sedation caused by antipsychotics, and certain antidepressants.[332]
Alcohol combined with cannabis (not to be confused with tincture of cannabis which contains minute quantities of alcohol) — known as cross-fading and may easily cause spins in people who are drunk and smoke potent cannabis; Ethanol increases plasma tetrahydrocannabinol levels, which suggests that ethanol may increase the absorption of tetrahydrocannabinol.[333]
TOMSO is a lesser-known psychedelic drug and a substituted amphetamine. TOMSO was first synthesized by Alexander Shulgin. According to Shulgin's book PiHKAL, TOMSO is inactive on its own and requires consumption of alcohol to become active.[334]
Hypnotics/sedatives

Alcohol can intensify the sedation caused by hypnotics/sedatives such as barbiturates, benzodiazepines, sedative antihistamines, opioids, nonbenzodiazepines/Z-drugs (such as zolpidem and zopiclone).[332]
Dextromethorphan
Combining alcohol with dextromethorphan significantly increases the risk of overdose and other severe health complications, according to the NIAAA.[335]
Disulfiram-like drugs
Disulfiram
Disulfiram inhibits the enzyme acetaldehyde dehydrogenase, which in turn results in buildup of acetaldehyde, a toxic metabolite of ethanol with unpleasant effects. The medication or drug is commonly used to treat alcohol use disorder, and results in immediate hangover-like symptoms upon consumption of alcohol, this effect is widely known as disulfiram effect.
Metronidazole
Metronidazole is an antibacterial agent that kills bacteria by damaging cellular DNA and hence cellular function.[336] Metronidazole is usually given to people who have diarrhea caused by Clostridioides difficile bacteria. Patients who are taking metronidazole are sometimes advised to avoid alcohol, even after 1 hour following the last dose. Although older data suggested a possible disulfiram-like effect of metronidazole, newer data has challenged this and suggests it does not actually have this effect.
Insulin
Alcohol consumption can cause hypoglycemia in diabetics on certain medications, such as insulin or sulfonylurea, by blocking gluconeogenesis.[337]
NSAIDs
The concomitant use of NSAIDs with alcohol and/or tobacco products significantly increases the already elevated risk of peptic ulcers during NSAID therapy.[338][better source needed]
The risk of stomach bleeding is still increased when aspirin is taken with alcohol or warfarin.[339][340]
Stimulants

Controlled animal and human studies showed that caffeine (energy drinks) in combination with alcohol increased the craving for more alcohol more strongly than alcohol alone.[341] These findings correspond to epidemiological data that people who consume energy drinks generally showed an increased tendency to take alcohol and other substances.[342][343]
Ethanol interacts with cocaine in vivo to produce cocaethylene, another psychoactive substance which may be substantially more cardiotoxic than either cocaine or alcohol by themselves.[344][345]
Ethylphenidate formation appears to be more common when large quantities of methylphenidate and alcohol are consumed at the same time, such as in non-medical use or overdose scenarios.[346] However, only a small percent of the consumed methylphenidate is converted to ethylphenidate.[347]
While nicotinis mimic the name of classic cocktails like the appletini (their name deriving from "martini"), combining nicotine with alcohol is a bad idea. Tobacco and nicotine actually heighten cravings for alcohol, making this a risky mix.[348]
Methanol and ethylene glycol
The rate-limiting steps for the elimination of ethanol are in common with certain other substances. As a result, the blood alcohol concentration can be used to modify the rate of metabolism of toxic alcohols, such as methanol and ethylene glycol. Methanol itself is not highly toxic, but its metabolites formaldehyde and formic acid are; therefore, to reduce the rate of production and concentration of these harmful metabolites, ethanol can be ingested.[349] Ethylene glycol poisoning can be treated in the same way.
Warfarin
Excessive use of alcohol is also known to affect the metabolism of warfarin and can elevate the INR, and thus increase the risk of bleeding.[350] The U.S. Food and Drug Administration (FDA) product insert on warfarin states that alcohol should be avoided.[351] The Cleveland Clinic suggests that when taking warfarin one should not drink more than "one beer, 6 oz of wine, or one shot of alcohol per day".[352]
Special population
Isoniazid
Levels of liver enzymes in the bloodstream should be frequently checked in daily alcohol drinkers, pregnant women, IV drug users, people over 35, and those who have chronic liver disease, severe kidney dysfunction, peripheral neuropathy, or HIV infection since they are more likely to develop hepatitis from INH.[353][354]
Pharmacology
Alcohol works in the brain primarily by increasing the effects of γ-Aminobutyric acid (GABA),[355] the major inhibitory neurotransmitter in the brain; by facilitating GABA's actions, alcohol suppresses the activity of the CNS.[355]
The pharmacology of ethanol involves both pharmacodynamics (how it affects the body) and pharmacokinetics (how the body processes it). In the body, ethanol primarily affects the central nervous system, acting as a depressant and causing sedation, relaxation, and decreased anxiety. The exact mechanism remains elusive, but ethanol has been shown to affect ligand-gated ion channels, particularly the GABAA receptor.
After oral ingestion, ethanol is absorbed via the stomach and intestines into the bloodstream. Ethanol is highly water-soluble and diffuses passively throughout the entire body, including the brain. Soon after ingestion, it begins to be metabolized, 90% or more by the liver. One standard drink is sufficient to almost completely saturate the liver's capacity to metabolize alcohol. The main metabolite is acetaldehyde, a toxic carcinogen. Acetaldehyde is then further metabolized into ionic acetate by the enzyme aldehyde dehydrogenase (ALDH). Acetate is not carcinogenic and has low toxicity,[356] but has been implicated in causing hangovers.[357][358] Acetate is further broken down into carbon dioxide and water and eventually eliminated from the body through urine and breath. 5 to 10% of ethanol is excreted unchanged in the breath, urine, and sweat.
Alcohol also direct affects a number of other neurotransmitter systems including those of glutamate, glycine, acetylcholine, and serotonin.[359][360] The pleasurable effects of alcohol ingestion are the result of increased levels of dopamine and endogenous opioids in the reward pathways of the brain.[361][362]
The average human digestive system produces approximately 3 g of ethanol per day through fermentation of its contents.[363]
Safety

Symptoms of ethanol overdose may include nausea, vomiting, CNS depression, coma, acute respiratory failure, or death. Levels of even less than 0.1% can cause intoxication, with unconsciousness often occurring at 0.3–0.4%.[332] Death from ethanol consumption is possible when blood alcohol levels reach 0.4%. A blood level of 0.5% or more is commonly fatal. The oral median lethal dose (LD50) of ethanol in rats is 5,628 mg/kg. Directly translated to human beings, this would mean that if a person who weighs 70 kg (150 lb) drank a 500 mL (17 US fl oz) glass of pure ethanol, they would theoretically have a 50% risk of dying. The highest blood alcohol level ever recorded, in which the subject survived, is 1.41%.[364]
A retrospective case-control study conducted from 1990 to 2001 found that alcohol consumption was responsible for over half of all deaths among Russian adults aged 15–54, significantly impacting mortality rates related to causes such as accidents, violence, and various diseases.[365]
In the US, the DEA has claimed illegal drugs are more deadly than alcohol, citing CDC data from 2000 showing similar death counts despite alcohol's wider use.[366] However, this comparison is disputed; a JAMA article reported alcohol-related deaths in 2000 as 85,000, significantly higher than the DEA's figure of 18,539.[367][368]
Toxicity
The WHO classifies alcohol as a toxic substance.[15] More specifically, ethanol is categorized as a cytotoxin,[369] hepatotoxin,[370] neurotoxin,[371] and ototoxin,[173] which has acute toxic effects on the cells, liver, the nervous system, and the ears, respectively. However, ethanol's acute effects on these organs are usually reversible. This means that even with a single episode of heavy drinking, the body can typically repair itself from the initial damage. Methanol laced alcohol on the other hand can cause blindness even in small quantities.
Ethanol is nutritious but highly intoxicating for most animals, which typically tolerate only up to 4% in their diet. However, a 2024 study found that oriental hornets fed sugary solutions containing 1% to 80% ethanol for a week showed no adverse effects on behavior or lifespan.[372]
- Margin of exposure of acute toxicity of various psychoactive drugs, visualized on a spectrum. The scale corresponds
Chemistry
Ethanol is also known chemically as alcohol, ethyl alcohol, or drinking alcohol. It is a simple alcohol with a molecular formula of C2H6O and a molecular weight of 46.0684 g/mol. The molecular formula of ethanol may also be written as CH3−CH2−OH or as C2H5−OH. The latter can also be thought of as an ethyl group linked to a hydroxyl (alcohol) group and can be abbreviated as EtOH. Ethanol is a volatile, flammable, colorless liquid with a slight characteristic odor. Aside from its use as a psychoactive and recreational substance, ethanol is also commonly used as an antiseptic and disinfectant, a chemical and medicinal solvent, and a fuel.
Production
Ethanol is produced naturally as a byproduct of the metabolic processes of yeast and hence is present in any yeast habitat, including even endogenously in humans, but it does not cause raised blood alcohol content as seen in the rare medical condition auto-brewery syndrome (ABS). It is manufactured through hydration of ethylene or by brewing via fermentation of sugars with yeast (most commonly Saccharomyces cerevisiae). The sugars are commonly obtained from sources like steeped cereal grains (e.g., barley), grape juice, and sugarcane products (e.g., molasses, sugarcane juice). Ethanol–water mixture which can be further purified via distillation.
Home-made alcoholic beverages
Homebrewing

Homebrewing is the brewing of beer or other alcoholic beverages on a small scale for personal, non-commercial purposes. Supplies, such as kits and fermentation tanks, can be purchased locally at specialty stores or online. Beer was brewed domestically for thousands of years before its commercial production, although its legality has varied according to local regulation. Homebrewing is closely related to the hobby of home distillation, the production of alcoholic spirits for personal consumption; however home distillation is generally more tightly regulated.
Moonshine
Although methanol is not produced in toxic amounts by fermentation of sugars from grain starches,[373] it is a major occurrence in fruit spirits.[374] However, in modern times, reducing methanol with the absorption of a molecular sieve is a practical method for production.[375]
Analogues

Ethanol has a variety of analogues, many of which have similar actions and effects. In chemistry, "alcohol" can encompass other mind-altering alcohols besides the kind we drink. Some examples include synthetic drugs like ethchlorvynol and methylpentynol, once used in medicine. Also, ethanol is colloquially referred to as "alcohol" because it is the most prevalent alcohol in alcoholic beverages. But technically all alcoholic beverages contain several types of psychoactive alcohols, that are categorized as primary, secondary, or tertiary. Primary, and secondary alcohols, are oxidized to aldehydes, and ketones, respectively, while tertiary alcohols are generally resistant to oxidation.[376] Ethanol is a primary alcohol that has unpleasant actions in the body, many of which are mediated by its toxic metabolite acetaldehyde.[377] Less prevalent alcohols found in alcoholic beverages, are secondary, and tertiary alcohols. For example, the tertiary alcohol 2M2B which is up to 50 times more potent than ethanol and found in trace quantities in alcoholic beverages, has been synthesized and used as a designer drug. Alcoholic beverages are sometimes laced with toxic alcohols, such as methanol (the simplest alcohol) and isopropyl alcohol.[16] A mild, brief exposure to isopropyl alcohol (which is only moderately more toxic than ethanol) is unlikely to cause any serious harm. But many methanol poisoning incidents have occurred through history, since methanol is lethal even in small quantities, as little as 10–15 milliliters (2–3 teaspoons). Ethanol is used to treat methanol and ethylene glycol toxicity.
The Lucas test differentiates between primary, secondary, and tertiary alcohols.
Society and culture
Evolving alcohol norms
Alcohol education
Alcohol education is the planned provision of information and skills relevant to living in a world where alcohol is commonly misused.[378] The World Health Organisations (WHO) Global Status Report on Alcohol and Health, highlights the fact that alcohol will be a larger problem in later years, with estimates suggesting it will be the leading cause of disability and death.[379] Informing people on alcohol and harmful drinking should become a priority.
Denormalization
In October 2024, the WHO Regional Office for Europe has launched the "Redefine alcohol" campaign to address alcohol-related health risks, as alcohol causes nearly 1 in 11 deaths in the region. The campaign aims to raise awareness about alcohol's link to over 200 diseases, including several cancers, and to encourage healthier choices by sharing research and personal stories. It also calls for stricter regulation of alcohol to reduce its societal harm. This initiative is part of the WHO/EU Evidence into Action Alcohol Project, which seeks to reduce alcohol-related harm across Europe.[380]
Intermittent sobriety
Intermittent sobriety refers to planned periods of abstinence from alcohol, often as part of awareness campaigns or personal health initiatives.[381][382]
Notable examples include:
- Dry January: An annual campaign encouraging people to abstain from alcohol for the month of January.
- Dry July: A similar initiative held in July, often with a fundraising component for cancer-related charities.
- Ocsober: An October-based challenge to abstain from alcohol.
Sober curious
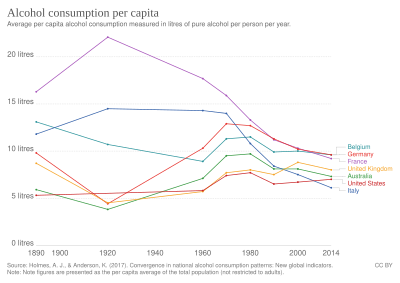
Sober curious is a cultural movement and lifestyle of consuming no or limited alcohol that started in the late 2010s.[citation needed] It differs from traditional abstinence in that it is not founded on asceticism, religious condemnation of alcohol or previous alcohol abuse, but motivated by a curiosity of a sober lifestyle. Markets have reacted by offering a wider selection of non-alcoholic beverages.[383]
Sober curiosity is often defined as having the option to question or change one's drinking habits, for mental or physical health reasons.[384] It may be practised in many ways, ranging from complete abstinence to more thought about when and how much is consumed.[385]
Since the onset of the COVID-19 pandemic, more people in Europe have reduced their alcohol consumption.[386]
Usage
Consumption recommendations

The recommended maximum intake (or safe limits) of alcohol varies from no intake, to daily, weekly, or daily/weekly guidelines provided by health agencies of governments. The World Health Organization published a statement in The Lancet Public Health in April 2023 that "there is no safe amount that does not affect health".[15]
According to the U.S. Department of Agriculture, based on NHANES 2013–2014 surveys, women in the US ages 20 and up consume on average 6.8 grams/day and men consume on average 15.5 grams/day.[387] A March 2023 review found light-moderate daily drinking not significantly associated with increased mortality rate, but higher intake raises risk, with women affected at lower levels than men.[388] However, according to a 2024 systematic review and meta-analysis, even at 20 g/day (1 large beer), the risk of developing an alcohol use disorder (AUD) is nearly 3 times higher than non-drinkers, and the risk of dying from an AUD is about 2 times higher than non-drinkers.[389]
Drinking culture

Ethanol is typically consumed as a recreational substance by mouth in the form of alcoholic beverages such as beer, wine, and spirits. It is commonly used in social settings due to its capacity to enhance sociability.
Drinking alcohol is generally socially acceptable and is legal in most countries, unlike with many other recreational substances. Many students attending colleges, universities, and other higher education institutions consume alcoholic beverages. However, there are often restrictions on alcohol sale and use, for instance a minimum age for drinking and laws against public drinking and drinking and driving.[390] A 2024 meta-analysis found that alcohol consumption increased on average each year, with the most significant rise occurring between the ages of 12 and 13. Drinking peaked around 22 years old, then began to decline at 24.[391]
Alcohol holds considerable societal and cultural significance, playing a role in social interactions across much of the world. Drinking establishments, such as bars and nightclubs, revolve primarily around the sale and consumption of alcoholic beverages, and parties, festivals, and social gatherings commonly involve alcohol consumption. Alcohol is related to various societal problems, including drunk driving, accidental injuries, sexual assaults, domestic abuse, and violent crime.[146] Alcohol remains illegal for sale and consumption in a number of countries, mainly in the Middle East.
Research on the societal benefits of alcohol is rare, but a 2017 study suggested there it was beneficial.[392] Alcohol is often used as a social lubricant; it increases occurrences of Duchenne smiling, talking, and social bonding, even when participants are unaware of their alcohol consumption or lack thereof.[393] In a study of the UK, regular drinking was correlated with happiness, feeling that life was worthwhile, and life satisfaction. According to a causal path analysis the cause was vice versa; alcohol consumption was not the cause, but rather that the life satisfaction resulted in greater happiness and an inclination to visit pubs and develop a regular drinking venue. City centre bars were distinguished by their focus on maximizing alcohol sales. Community pubs had less variation in visible group sizes and longer, more focused conversations than those in city centre bars. Drinking regularly at a community pub led to higher trust in others and better networking with the local community, compared to non-drinkers and city centre bar drinkers.[392]
Global initiatives
United Nations Sustainable Development Goal 3 is part of "The Alcohol Policy Playbook," which is a resource for reaching the goals of the WHO European Framework for Action on Alcohol (2022–2025) and the WHO Global Alcohol Action Plan (2022–2030).[394]
Psychosocial factors
Research has shown that various psychosocial factors can influence alcohol consumption patterns throughout an individual's life.
A 2024 study from UT Southwestern Medical Center indicates that higher IQ during high school is linked to a greater likelihood of moderate or heavy drinking in midlife, with each one-point increase in IQ correlating to a 1.6% higher probability of such drinking. The study also found that this relationship is influenced by psychosocial factors, particularly income and career stress, highlighting the need for further research in diverse populations.[395][396]
Religion

The relationship between religion and alcohol exhibits variations across cultures, geographical areas, and religious denominations. Some religions emphasize moderation and responsible use as a means of honoring the divine gift of life, while others impose outright bans on alcohol as a means of honoring the divine gift of life. Moreover, within the same religious tradition, there are many adherents that may interpret and practice their faith's teachings on alcohol in diverse ways. Hence, a wide range of factors, such as religious affiliation, levels of religiosity, cultural traditions, family influences, and peer networks, collectively influence the dynamics of this relationship.
The levels of alcohol use in spiritual context can be broken down into:
- Prohibition: Some religions, including Islam[397] prohibit alcohol consumption.
- Symbolic use: In some Christian denominations, the sacramental wine is alcoholic, however, only a sip is taken, and it does not raise the blood alcohol content, and other denominations are using nonalcoholic wine. See also Libation.
- Discourage consumption: Hinduism does not have a central authority which is followed by all Hindus, though religious texts generally discourage the use or consumption of alcohol.
- Inebriating spiritual use: See the spiritual section.
Secularity
In some cultures, including those with religious traditions, consuming alcohol in moderation to celebrate joyful occasions is accepted in a non-religious, secular context.
During the Jewish holiday of Purim, Jews are obligated to drink (especially Kosher wine) until their judgmental abilities become impaired according to the Book of Esther.[398][399][400] However, Purim has more of a national than a religious character.
Misconceptions
While the terms "drug" and "medicine" are sometimes used interchangeably, "drug" can have a negative connotation, often associated with illegal substances like cocaine or heroin.[401] Criticism of the alcohol industry may note that the industry argues that "alcohol is not a drug".[402][403] However, the term "Alcohol and Other Drugs" emphasizes this inclusion by grouping alcohol with other substances that alter mood and behavior.
The term narcotic usually refers to opiates or opioids, which are called narcotic analgesics. In common parlance and legal usage, it is often used imprecisely to mean illicit drugs, irrespective of their pharmacology.[404] However, in countries with alcohol prohibition, it is classified and treated as a narcotic. Also, research acknowledges that alcohol can have similar effects to narcotics in head and/or trunk trauma situations.[405] In addition to these findings, recent research indicates that among chronic pain patients on long-term opioid therapy, alcohol consumption is connected to heightened opioid cravings.[406]
The normalization of alcohol consumption,[407] along with past misconceptions about its health benefits, also promoted by the industry,[408] further reinforces the mistaken idea that it is not a "drug". Even within the realm of scientific inquiry, the common phrase "drugs and alcohol" persists, implying that alcohol is somehow separate from other drugs.
Paradoxically, despite being legal, alcohol, scientifically classified as a drug, has demonstrably been linked to greater social harm than most illegal drugs.[215][216] This contradicts the perception some hold of alcohol being a harmless substance.
Law
Legal status

Alcohol consumption is fully legal and available in most countries of the world.[409] Home made alcoholic beverages with low alcohol content like wine, and beer is also legal in most countries, but distilling moonshine outside of a registered distillery remains illegal in most of them.
Some majority-Muslim countries, such as Saudi Arabia, Kuwait, Pakistan, Iran and Libya prohibit the production, sale, and consumption of alcoholic beverages because they are forbidden by Islam.[410][411][412] Laws banning alcohol consumption are found in some Indian states as well as some Native American reservations in the U.S.[409]
In addition, there are regulations on alcohol sales and use in many countries throughout the world.[409] For instance, the majority of countries have a minimum legal drinking age to purchase or consume alcoholic beverages, although there are often exceptions such as underage consumption of small amounts of alcohol with parental supervision. Also, some countries have bans on public intoxication.[409] Drinking while driving or intoxicated driving is frequently outlawed and it may be illegal to have an open container of alcohol or liquor bottle in an automobile, bus or aircraft.[409]
In Iran, consumption of alcohol (one glass) is punished by 80 lashes, but repeated offences may lead to death penalty, although rarely exercised. In 2012, two men were sentenced to death after a third offense in Khorasan.[413][414]
Alcohol packaging warning messages

Alcohol packaging warning messages (alcohol warning labels, AWLs[415]) are warning messages that appear on the packaging of alcoholic drinks concerning their health effects.
A World Health Organization report, published in 2017, stated:[416]
Alcohol product labelling could be considered as a component of a comprehensive public health strategy to reduce alcohol-related harm. Adding health labels to alcohol containers is an important first step in raising awareness and has a longer-term utility in helping to establish a social understanding of the harmful use of alcohol.
Minimum pricing policies
In 2018, Scotland became the first country to implement a minimum unit pricing policy for alcohol, setting the price at 50 pence per unit. This measure aimed to reduce alcohol-related harm by making cheap, high-strength alcohol less accessible. As of September 2024, the minimum price has increased to 65 pence per unit, reflecting efforts to address inflation and continue reducing alcohol-related deaths and hospital admissions.[417]
Austria, Switzerland and Germany determine that a barkeeper has to offer one or more non-alcoholic beverages at a cheaper price than any alcoholic drink. Before the so-called Apfelsaft-Paragraph (applejuice clause) was established in Germany in 2002 beer was often the cheapest beverage available.
Criticism of the alcohol industry

A 2019 survey conducted by the American Institute for Cancer Research (AICR) showed that only 45% of Americans were aware of the associated risk of cancer due to alcohol consumption, up from 39% in 2017.[418] The AICR believes that alcohol advertising about the healthy cardiovascular benefits of modest alcohol overshadow messages about the increased cancer risks.[418]
Drinking alcoholic beverages increase the risk for breast cancer. Several studies indicate that the use of marketing by the alcohol industry to associate their products with breast cancer awareness campaigns, known as pinkwashing, is misleading and potentially harmful.[419][420][421][422]
The alcohol industries have marketed products directly to the LGBT+ community. In 2010, of the sampled parades that listed sponsors, 61% of the prides were sponsored by the alcohol industry.[423] A study found that alcohol consumption within LGBTQ+ communities presents a challenge for health promotion efforts. The positive association with alcohol within these communities makes it harder to reduce alcohol-related health issues.[424]
Standard drink
A standard drink is a measure of alcohol consumption representing a fixed amount of pure ethanol, used in relation to recommendations about alcohol consumption and its relative risks to health. The size of a standard drink varies from 8g to 20g across countries, but 10g alcohol (12.7 millilitres) is used in the World Health Organization (WHO) Alcohol Use Disorders Identification Test (AUDIT)'s questionnaire form example,[425] and has been adopted by more countries than any other amount.[426]
History
The consumption of alcohol has a long human history. Beginning with the Gin Craze, excessive drinking and drunkenness developed into a major problem for public health.[427][428] Prohibition marked a turning point, as alcohol transitioned from widely accepted to strictly controlled, recognized as a dangerous drug. After its repeal, societal views softened dramatically. Alcohol consumption became normalized, and for many years, the public remained largely unaware of the well-established dangers, including its carcinogenic and teratogenic properties. However, a recent shift has brought these risks back to light. The WHO's 2023 declaration that no amount of alcohol consumption is entirely safe served as a wake-up call.
Ancient World
Since antiquity, prior to the development of modern agents, alcohol was used as a general anaesthetic.[429]
In the history of wound care, beer,[430] and wine,[431] are recognized as substances used for healing wounds.
Late Middle Ages
Alcohol has been used as an antiseptic as early as 1363 with evidence to support its use becoming available in the late 1800s.[citation needed]
Early modern period

The popular story dates the etymology of the term Dutch courage to English soldiers fighting in the Anglo-Dutch Wars[432] (1652–1674) and perhaps as early as the Thirty Years' War (1618–1648). One version states that jenever (or Dutch gin) was used by English soldiers for its calming effects before battle, and for its purported warming properties on the body in cold weather. Another version has it that English soldiers noted the bravery-inducing effects of jenever on Dutch soldiers.[433][434]
The Gin Craze was a period in the first half of the 18th century when the consumption of gin increased rapidly in Great Britain, especially in London. By 1743, England was drinking 2.2 gallons (10 litres) of gin per person per year. The Sale of Spirits Act 1750 (commonly known as the Gin Act 1751) was an Act of the Parliament of Great Britain (24 Geo. 2. c. 40) which was enacted to reduce the consumption of gin and other distilled spirits, a popular pastime[435] that was regarded as one of the primary causes of crime in London.[436]
Modern period

The rum ration (also called the tot) was a daily amount of rum given to sailors on Royal Navy ships. It started 1866 and was abolished in 1970 after concerns that the intake of strong alcohol would lead to unsteady hands when working machinery.
The Andrew Johnson alcoholism debate is the dispute, originally conducted among the general public, and now typically a question for historians, about whether or not Andrew Johnson, the 17th president of the United States (1865–1869), drank to excess.
The Bratt System was a system that was used in Sweden (1919–1955) and similarly in Finland (1944–1970) to control alcohol consumption, by rationing of liquor. Every citizen allowed to consume alcohol was given a booklet called a motbok (viinakortti in Finland), in which a stamp was added each time a purchase was made at Systembolaget (in Sweden) and Alko (in Finland).[437] A similar system also existed in Estonia between July 1, 1920 to December 31, 1925.[438] The stamps were based on the amount of alcohol bought. When a certain amount of alcohol had been bought, the owner of the booklet had to wait until next month to buy more.
The Medicinal Liquor Prescriptions Act of 1933 was a law passed by Congress in response to the abuse of medicinal liquor prescriptions during Prohibition.
Gilbert Paul Jordan (aka The Boozing Barber) was a Canadian serial killer who is believed to have committed the so-called "alcohol murders" between 1965–c. 2004 in Vancouver, British Columbia.
Alcohol as a gateway drug
Alcohol and nicotine prime the brain for a heightened response to other drugs and are, like marijuana, also typically used before a person progresses to other, more harmful substances."[439]
A study of drug use of 14,577 U.S. 12th graders showed that alcohol consumption was associated with an increased probability of later use of tobacco, cannabis, and other illegal drugs.[440]
See also
- Alcohol myopia
- Cannabis (drug)
- Glossary of alcohol (drug) terms
- Lean (drug)
- Rum-running
- Responsible drug use
- GABAergics
- GABRD (δ subunit-containing receptors)
- Pigovian taxes, which are to pay for the damage to society caused by these goods.
- Speedball (drug)
- Sin taxes are used to increase the price in an effort to lower their use, or failing that, to increase and find new sources of revenue.
References
- ^ WHO Expert Committee on Problems Related to Alcohol Consumption: second report. Geneva, Switzerland: World Health Organization. 2007. p. 23. ISBN 978-92-4-120944-1. Retrieved 3 March 2015.
...alcohol dependence (is) a substantial risk of regular heavy drinking...
- ^ Vengeliene V, Bilbao A, Molander A, Spanagel R (May 2008). "Neuropharmacology of alcohol addiction". British Journal of Pharmacology. 154 (2): 299–315. doi:10.1038/bjp.2008.30. PMC 2442440. PMID 18311194.
(Compulsive alcohol use) occurs only in a limited proportion of about 10–15% of alcohol users....
- ^ Gilman JM, Ramchandani VA, Crouss T, Hommer DW (January 2012). "Subjective and neural responses to intravenous alcohol in young adults with light and heavy drinking patterns". Neuropsychopharmacology. 37 (2): 467–77. doi:10.1038/npp.2011.206. PMC 3242308. PMID 21956438.
- ^ a b c d e f Principles of Addiction: Comprehensive Addictive Behaviors and Disorders. Academic Press. 17 May 2013. pp. 162–. ISBN 978-0-12-398361-9.
- ^ a b c Holford NH (November 1987). "Clinical pharmacokinetics of ethanol". Clinical Pharmacokinetics. 13 (5): 273–92. doi:10.2165/00003088-198713050-00001. PMID 3319346. S2CID 19723995.
- ^ a b c d Pohorecky LA, Brick J (1988). "Pharmacology of ethanol". Pharmacology & Therapeutics. 36 (2–3): 335–427. doi:10.1016/0163-7258(88)90109-x. PMID 3279433.
- ^ Becker CE (September 1970). "The clinical pharmacology of alcohol". California Medicine. 113 (3): 37–45. PMC 1501558. PMID 5457514.
- ^ a b Levine B (2003). Principles of Forensic Toxicology. Amer. Assoc. for Clinical Chemistry. pp. 161–. ISBN 978-1-890883-87-4.
- ^ Iber FL (26 November 1990). Alcohol and Drug Abuse as Encountered in Office Practice. CRC Press. pp. 74–. ISBN 978-0-8493-0166-7.
- ^ a b c Haynes WM, ed. (2011). CRC Handbook of Chemistry and Physics (92nd ed.). Boca Raton, FL: CRC Press. p. 3.246. ISBN 1-4398-5511-0.
- ^ "The Origin Of The Word 'Alcohol'". Science Friday. Retrieved 30 September 2024.
- ^ Song F, Walker MP (8 November 2023). "Sleep, alcohol, and caffeine in financial traders". PLOS ONE. 18 (11): e0291675. Bibcode:2023PLoSO..1891675S. doi:10.1371/journal.pone.0291675. PMC 10631622. PMID 37939019.
- ^ "Medscape: Medscape Access". medscape.com. 16 October 2021.
- ^ Costardi JV, Nampo RA, Silva GL, Ribeiro MA, Stella HJ, Stella MB, et al. (August 2015). "A review on alcohol: from the central action mechanism to chemical dependency". Revista da Associacao Medica Brasileira. 61 (4): 381–387. doi:10.1590/1806-9282.61.04.381. PMID 26466222.
- ^ a b c d e f g "No level of alcohol consumption is safe for our health". World Health Organization. 4 January 2023.
- ^ a b Collins SE, Kirouac M (2013). "Alcohol Consumption". Encyclopedia of Behavioral Medicine. Springer. pp. 61–65. doi:10.1007/978-1-4419-1005-9_626. ISBN 978-1-4419-1004-2.
- ^ Różański M, Pielech-Przybylska K, Balcerek M (September 2020). "Influence of Alcohol Content and Storage Conditions on the Physicochemical Stability of Spirit Drinks". Foods. 9 (9): 1264. doi:10.3390/foods9091264. PMC 7555269. PMID 32916918.
- ^ a b Madrid P (March 1992). "Wrath of Grapes". This Rock. 3 (3). Archived from the original on 7 March 2007. Retrieved 16 March 2007.
The [Catholic] Church teaches ... that wine, like food, sex, laughter, and dancing, is a good thing when enjoyed in its proper time and context. To abuse any good thing is a sin, but the thing abused does not itself become sinful.
- ^ a b "Agents Classified by the IARC Monographs, Volumes 1–111" (PDF). Archived from the original (PDF) on 25 October 2011 – via monographs.iarc.fr.
- ^ a b Griswold MG, Fullman N, Hawley C, Arian N, Zimsen SR, Tymeson HD, et al. (September 2018). "Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016". Lancet. 392 (10152): 1015–1035. doi:10.1016/S0140-6736(18)31310-2. PMC 6148333. PMID 30146330.
- ^ a b c Global status report on alcohol and health (PDF). World Health Organization. 2018. ISBN 978-92-4-156563-9.
- ^ "Over 3 million annual deaths due to alcohol and drug use, majority among men". wwho.int.
- ^ "Canada's Guidance on Alcohol and Health". ccsa.ca. Archived from the original on 11 September 2023. Retrieved 25 September 2023.
- ^ "Empfehlungen zum Umgang mit Alkohol" (PDF). Deutsche Hauptstelle für Suchtfragen (in German). Archived (PDF) from the original on 24 October 2023. Retrieved 30 October 2023.
- ^ "What Are the U.S. Guidelines for Drinking? - Rethinking Drinking | NIAAA". rethinkingdrinking.niaaa.nih.gov.
- ^ Mégarbane B (24 August 2010). "Treatment of patients with ethylene glycol or methanol poisoning: focus on fomepizole". Open Access Emergency Medicine. 2: 67–75. doi:10.2147/OAEM.S5346. PMC 4806829. PMID 27147840.
- ^ British National Formulary: BNF 69 (69th ed.). British Medical Association. 2015. pp. 42, 838. ISBN 978-0-85711-156-2.
- ^ Barceloux DG, Bond GR, Krenzelok EP, Cooper H, Vale JA (2002). "American Academy of Clinical Toxicology practice guidelines on the treatment of methanol poisoning". Journal of Toxicology. Clinical Toxicology. 40 (4): 415–46. doi:10.1081/CLT-120006745. PMID 12216995. S2CID 26495651.
- ^ "Our 'drinking culture' explored". www.linkedin.com. Retrieved 25 January 2024.
- ^ "Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings" (PDF). United States Substance Abuse and Mental Health Services Administration. United States Department of Health and Human Services. Retrieved 11 June 2015.
- ^ Renaud SC (2001). "Diet and stroke". The Journal of Nutrition, Health & Aging. 5 (3): 167–172. PMID 11458287.
- ^ Nyberg ST, Batty GD, Pentti J, Madsen IE, Alfredsson L, Bjorner JB, et al. (August 2022). "Association of alcohol use with years lived without major chronic diseases: A multicohort study from the IPD-Work consortium and UK Biobank". The Lancet Regional Health. Europe. 19: 100417. doi:10.1016/j.lanepe.2022.100417. PMC 9160494. PMID 35664051.
- ^ Perez-Araluce R, Bes-Rastrollo M, Martínez-González MÁ, Toledo E, Ruiz-Canela M, Barbería-Latasa M, et al. (February 2023). "Effect of Binge-Drinking on Quality of Life in the 'Seguimiento Universidad de Navarra' (SUN) Cohort". Nutrients. 15 (5): 1072. doi:10.3390/nu15051072. PMC 10004732. PMID 36904072.
- ^ Wakabayashi KT, Greeman EA, Barrett ST, Bevins RA (September 2021). "The Sugars in Alcohol Cocktails Matter". ACS Chemical Neuroscience. 12 (18): 3284–3287. doi:10.1021/acschemneuro.1c00526. PMC 8447180. PMID 34428024.
- ^ a b "Drinking Levels and Patterns Defined | National Institute on Alcohol Abuse and Alcoholism (NIAAA)". www.niaaa.nih.gov.
- ^ Snetselaar LG, de Jesus JM, DeSilva DM, Stoody EE (November 2021). "Dietary Guidelines for Americans, 2020-2025: Understanding the Scientific Process, Guidelines, and Key Recommendations". Nutrition Today. 56 (6): 287–295. doi:10.1097/NT.0000000000000512. PMC 8713704. PMID 34987271.
- ^ Snetselaar LG, de Jesus JM, DeSilva DM, Stoody EE (November 2021). "Dietary Guidelines for Americans, 2020-2025: Understanding the Scientific Process, Guidelines, and Key Recommendations". Nutrition Today. 56 (6): 287–295. doi:10.1097/NT.0000000000000512. PMC 8713704. PMID 34987271.
- ^ a b "NHIS - Adult Alcohol Use - Glossary". www.cdc.gov. 10 May 2019.
- ^ Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, et al. (February 2015). "Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis". British Journal of Cancer. 112 (3): 580–593. doi:10.1038/bjc.2014.579. PMC 4453639. PMID 25422909.
- ^ Caprio GG, Picascia D, Dallio M, Vitiello PP, Giunta EF, De Falco V, et al. (2020). "Light Alcohol Drinking and the Risk of Cancer Development: A Controversial Relationship". Reviews on Recent Clinical Trials. 15 (3): 164–177. doi:10.2174/1574887115666200628143015. PMID 32598271.
- ^ de Menezes RF, Bergmann A, Thuler LC (2013). "Alcohol consumption and risk of cancer: a systematic literature review". Asian Pacific Journal of Cancer Prevention. 14 (9): 4965–4972. doi:10.7314/apjcp.2013.14.9.4965. PMID 24175760.
- ^ a b Gormley M, Creaney G, Schache A, Ingarfield K, Conway DI (November 2022). "Reviewing the epidemiology of head and neck cancer: definitions, trends and risk factors". British Dental Journal. 233 (9): 780–786. doi:10.1038/s41415-022-5166-x. PMC 9652141. PMID 36369568.
- ^ Yasinski E (12 January 2021). "Even If You Don't Drink Daily, Alcohol Can Mess With Your Brain". Discover.
- ^ a b Maani Hessari N, Petticrew M (March 2018). "What does the alcohol industry mean by 'Responsible drinking'? A comparative analysis". Journal of Public Health. 40 (1). Oxford, England: 90–97. doi:10.1093/pubmed/fdx040. PMID 28398571.
- ^ "Definition of SOCIAL DRINKER". Merriam-Webster. Retrieved 2 April 2024.
- ^ Neal DJ, Fromme K (November 2007). "Hook 'em horns and heavy drinking: alcohol use and collegiate sports". Addictive Behaviors. 32 (11): 2681–2693. doi:10.1016/j.addbeh.2007.06.020. PMC 2527738. PMID 17662537.
- ^ Dumbili EW (January 2022). "'I just drink to feel abnormal for some time': Reconfiguring heavy drinking and intoxication as pleasurable". The International Journal on Drug Policy. 99: 103454. doi:10.1016/j.drugpo.2021.103454. PMID 34537478.
- ^ "NHIS - Adult Alcohol Use - Glossary". 10 May 2019.
- ^ Esser MB, Hedden SL, Kanny D, Brewer RD, Gfroerer JC, Naimi TS (November 2014). "Prevalence of alcohol dependence among US adult drinkers, 2009–2011". Preventing Chronic Disease. 11: E206. doi:10.5888/pcd11.140329. PMC 4241371. PMID 25412029.
- ^ Gable RS (June 2004). "Comparison of acute lethal toxicity of commonly abused psychoactive substances" (PDF). Addiction. 99 (6): 686–96. doi:10.1111/j.1360-0443.2004.00744.x. PMID 15139867.
- ^ Riley JL 3rd, King C (September 2009). "Self-report of alcohol use for pain in a multi-ethnic community sample". The Journal of Pain. 10 (9): 944–52. doi:10.1016/j.jpain.2009.03.005. PMC 2734914. PMID 19712901.
- ^ Carrigan MH, Randall CL (March 2003). "Self-medication in social phobia: a review of the alcohol literature". Addictive Behaviors. 28 (2): 269–284. doi:10.1016/S0306-4603(01)00235-0. PMC 6683821. PMID 12573678. Archived from the original on 31 January 2018. Retrieved 5 April 2024.
- ^ Wetterling T, Junghanns K (December 2000). "Psychopathology of alcoholics during withdrawal and early abstinence". European Psychiatry. 15 (8): 483–488. doi:10.1016/S0924-9338(00)00519-8. PMID 11175926. S2CID 24094651.
- ^ Cowley DS (January 1992). "Alcohol abuse, substance abuse, and panic disorder". The American Journal of Medicine. 92 (1A): 41S–48S. doi:10.1016/0002-9343(92)90136-Y. PMID 1346485.
- ^ Cosci F, Schruers KR, Abrams K, Griez EJ (June 2007). "Alcohol use disorders and panic disorder: a review of the evidence of a direct relationship". The Journal of Clinical Psychiatry. 68 (6): 874–880. doi:10.4088/JCP.v68n0608. PMID 17592911.
- ^ Müller CP, Schumann G, Rehm J, Kornhuber J, Lenz B (July 2023). "Self-management with alcohol over lifespan: psychological mechanisms, neurobiological underpinnings, and risk assessment". Molecular Psychiatry. 28 (7): 2683–2696. doi:10.1038/s41380-023-02074-3. PMC 10615763. PMID 37117460.
- ^ Ferguson E, Fiore A, Yurasek AM, Cook RL, Boissoneault J (February 2023). "Association of therapeutic and recreational reasons for alcohol use with alcohol demand". Experimental and Clinical Psychopharmacology. 31 (1): 106–115. doi:10.1037/pha0000554. PMC 9399303. PMID 35201830.
- ^ "Myth busters". who.int. World Health Organization.
- ^ "Is drinking alcohol part of a healthy lifestyle?". American Heart Association. 2020.
- ^ Bhandari S (ed.). "Alcohol & Sleep: Nix the Nightcap?". Webmd. Retrieved 1 November 2015.
- ^ Penning R, van Nuland M, Fliervoet LA, Olivier B, Verster JC (June 2010). "The pathology of alcohol hangover". Current Drug Abuse Reviews. 3 (2): 68–75. doi:10.2174/1874473711003020068. PMID 20712596.
- ^ Wiese JG, Shlipak MG, Browner WS (June 2000). "The alcohol hangover". Annals of Internal Medicine. 132 (11): 897–902. doi:10.7326/0003-4819-132-11-200006060-00008. PMID 10836917.
- ^ Breene S (6 October 2016). "The best and worst foods to cure a hangover". The Atlanta Journal-Constitution. Retrieved 30 July 2017.
- ^ Acocella J (26 May 2008). "A Few Too Many: Is there any hope for the hung over?". The New Yorker.
- ^ Harding A (21 December 2010). "10 Hangover Remedies: What Works?". Health.com. Retrieved 30 July 2017.
- ^ Howard J (17 March 2017). "What to eat to beat a hangover". CNN. Retrieved 30 July 2017.
- ^ Szabo G, Saha B (2015). "Alcohol's Effect on Host Defense". Alcohol Research. 37 (2): 159–170. PMC 4590613. PMID 26695755.
- ^ Kimmel M (2008). Guyland. New York: Harper. ISBN 978-0-06-083134-9.
- ^ Klein J (11 February 2022). "Dry dating: The rise of sober love and sex". www.bbc.com.
- ^ McAlpine D (7 November 2011). "The Secret to Great Dating This Winter? Cut The Booze". HuffPost UK.
- ^ Thompson SJ (10 January 2019). "Trend for sober dating sees an increase as singles seek love during Dry January". Daily Record.
- ^ Yang C, Latkin C, Luan R, Nelson K (February 2013). "Factors associated with drinking alcohol before visiting female sex workers among men in Sichuan Province, China". AIDS and Behavior. 17 (2): 568–573. doi:10.1007/s10461-012-0260-8. PMC 4017933. PMID 22806054.
- ^ a b Beksinska A, Karlsen O, Gafos M, Beattie TS (2023). "Alcohol use and associated risk factors among female sex workers in low- and middle-income countries: A systematic review and meta-analysis". PLOS Global Public Health. 3 (6): e0001216. doi:10.1371/journal.pgph.0001216. PMC 10263362. PMID 37310993.
- ^ Malatesta VJ, Pollack RH, Crotty TD, Peacock LJ (February 1982). "Acute Alcohol Intoxication and Female Orgasmic Response". The Journal of Sex Research. 18 (1): 1–17. doi:10.1080/00224498209551130. JSTOR 3812507.
- ^ Jones E, Fear NT (April 2011). "Alcohol use and misuse within the military: a review". International Review of Psychiatry. 23 (2): 166–172. doi:10.3109/09540261.2010.550868. PMID 21521086.
- ^ Dworkin ER, Bergman HE, Walton TO, Walker DD, Kaysen DL (2018). "Co-Occurring Post-Traumatic Stress Disorder and Alcohol Use Disorder in U.S. Military and Veteran Populations". Alcohol Research. 39 (2): 161–169. PMC 6561402. PMID 31198655.
- ^ Richardson JD, St Cyr KC, McIntyre-Smith AM, Haslam D, Elhai JD, Sareen J (August 2012). "Examining the association between psychiatric illness and suicidal ideation in a sample of treatment-seeking Canadian peacekeeping and combat veterans with posttraumatic stress disorder PTSD". Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie. 57 (8): 496–504. doi:10.1177/070674371205700808. PMID 22854032.
- ^ Kalinowski K (21 July 2023). "Rosyjska armia pije na potęgę. To jeden z głównych powodów wysokiej śmiertelności wojsk Putina na froncie" [The Russian army drinks heavily. This is one of the main reasons for the high mortality of Putin's troops at the front]. Gazeta Wyborcza (in Polish). Retrieved 24 July 2023.
- ^ Hambling D. "Are Drugs Making Russian Soldiers Act Like Zombies?". Forbes. Retrieved 24 July 2023.
- ^ Lister T, Pleitgen F, Hak K (1 February 2023). "Fighting Wagner is like a 'zombie movie' says Ukrainian soldier". CNN. Retrieved 24 July 2023.
- ^ "Ukrainians warn of 'drug-fuelled' Russian 'zombie waves' on the frontline". Forces Network. 1 March 2023. Retrieved 24 July 2023.
- ^ "Composition of Foods Raw, Processed, Prepared USDA National Nutrient Database for Standard Reference, Release 26 Documentation and User Guide" (PDF). USDA. August 2013. p. 14. Archived (PDF) from the original on 25 September 2014. Retrieved 3 February 2014.
- ^ Metz R, Berger S, Mako M (August 1969). "Potentiation of the plasma insulin response to glucose by prior administration of alcohol. An apparent islet-priming effect" (PDF). Diabetes. 18 (8): 517–522. doi:10.2337/diab.18.8.517. PMID 4897290. S2CID 32072796. Archived (PDF) from the original on 22 February 2014. Retrieved 11 February 2014.
- ^ Shelmet JJ, Reichard GA, Skutches CL, Hoeldtke RD, Owen OE, Boden G (April 1988). "Ethanol causes acute inhibition of carbohydrate, fat, and protein oxidation and insulin resistance". The Journal of Clinical Investigation. 81 (4): 1137–1145. doi:10.1172/JCI113428. PMC 329642. PMID 3280601.
- ^ Leeds JS, Oppong K, Sanders DS (May 2011). "The role of fecal elastase-1 in detecting exocrine pancreatic disease". Nature Reviews. Gastroenterology & Hepatology. 8 (7): 405–415. doi:10.1038/nrgastro.2011.91. PMID 21629239.
- ^ Osborne VA, Sher KJ, Winograd RP (2011). "Disordered eating patterns and alcohol misuse in college students: Evidence for "drunkorexia"?". Comprehensive Psychiatry. 52 (6): e12. doi:10.1016/j.comppsych.2011.04.038.
- ^ "'Drunkorexia:' A Recipe for Disaster". ScienceDaily. 17 October 2011.
- ^ Kopelman MD, Thomson AD, Guerrini I, Marshall EJ (2009). "The Korsakoff syndrome: clinical aspects, psychology and treatment". Alcohol and Alcoholism. 44 (2): 148–154. doi:10.1093/alcalc/agn118. PMID 19151162.
- ^ O'Callaghan P (March 1992). "The Spirit of True Christianity". Word Magazine. Antiochian Orthodox Christian Archdiocese of North America: 8–9. Retrieved 16 March 2007.
So alcohol, sex, the body, money, television, and music are all good things. It is only the abuse of these things that is bad—drunkenness, pornography, compulsive gambling, etc. Even drugs marijuana, cocaine, heroin—all have good uses for medical and other reasons. It's only the abuse of them for pleasure that is wrong.
- ^ Ethical Investment Advisory Group (January 2005). "Alcohol: An inappropriate investment for Anglicanism" (PDF). Church of England. Archived from the original (PDF) on 26 February 2007. Retrieved 8 February 2007.
Christians who are committed to total abstinence have sometimes interpreted biblical references to wine as meaning unfermented grape juice, but this is surely inconsistent with the recognition of both good and evil in the biblical attitude to wine. It is self-evident that human choice plays a crucial role in the use or abuse of alcohol.
- ^ "Responding to Opportunities for 'Interim Eucharistic Sharing'" (PDF). Evangelical Lutheran Church in America. Archived from the original (PDF) on 14 February 2007. Retrieved 24 February 2007.
While many Lutheran congregations also provide grape juice or unfermented wine as an alternative, Lutherans have more emphasized the historical and ecumenical continuities which wine provides, as well as the richness and multivalences of its symbolic associations.
- ^ "Theology and Practice of The Lord's Supper - Part I" (PDF). Lutheran Church–Missouri Synod. May 1983. Retrieved 24 February 2007.
- ^ "Alcohol". Presbyterian 101. Presbyterian Church (USA). Archived from the original on 13 April 2003. Retrieved 24 February 2007.
- ^ "Introduction to Worship in the United Church of Christ" (PDF). Book of Worship. United Church of Christ. 1986. pp. Footnote 27. Archived from the original (PDF) on 8 June 2012. Retrieved 24 February 2007.
- ^ "Alcohol". Christian Reformed Church in North America. 1996–2007. Archived from the original on 21 October 2012. Retrieved 24 February 2007.
- ^ "Alcohol, Beverage use of". Presbyterian Church in America, 8th General Assembly. 1980. Archived from the original on 12 September 2017. Retrieved 24 February 2007.
- ^ "Maintain a Balanced View Of Alcohol". Watch Tower Bible and Tract Society of Pennsylvania. 2004. Retrieved 24 November 2012.
- ^ Soileau M (August 2012). "Spreading the Sofra: Sharing and Partaking in the Bektashi Ritual Meal". History of Religions. 52 (1): 1–30. doi:10.1086/665961. JSTOR 10.1086/665961. Retrieved 5 June 2021.
- ^ Bocking B (1997). A popular dictionary of Shintō (Rev. ed.). Richmond, Surrey [U.K.]: Curzon Press. ISBN 0-7007-1051-5. OCLC 264474222.
- ^ "Civil Commitment: About This Policy". Alcohol Policy Information System. NIAAA. Retrieved 15 March 2024.
- ^ Popova S, Dozet D, Shield K, Rehm J, Burd L (September 2021). "Alcohol's Impact on the Fetus". Nutrients. 13 (10): 3452. doi:10.3390/nu13103452. PMC 8541151. PMID 34684453.
- ^ Chung DD, Pinson MR, Bhenderu LS, Lai MS, Patel RA, Miranda RC (August 2021). "Toxic and Teratogenic Effects of Prenatal Alcohol Exposure on Fetal Development, Adolescence, and Adulthood". International Journal of Molecular Sciences. 22 (16): 8785. doi:10.3390/ijms22168785. PMC 8395909. PMID 34445488.
- ^ "Facts about FASDs". 16 April 2015. Archived from the original on 23 May 2015. Retrieved 10 June 2015.
- ^ "More than 3 million US women at risk for alcohol-exposed pregnancy". Centers for Disease Control and Prevention. 2 February 2016. Retrieved 3 March 2016.
'drinking any alcohol at any stage of pregnancy can cause a range of disabilities for their child,' said Coleen Boyle, Ph.D., director of CDC's National Center on Birth Defects and Developmental Disabilities.
- ^ Riley EP, Infante MA, Warren KR (June 2011). "Fetal alcohol spectrum disorders: an overview". Neuropsychology Review. 21 (2): 73–80. doi:10.1007/s11065-011-9166-x. PMC 3779274. PMID 21499711.
- ^ Oliver A, Overton C (May 2014). "Diagnosis and management of miscarriage". The Practitioner. 258 (1771): 25–8, 3. PMID 25055407.
- ^ Van Nguyen JM, Abenhaim HA (October 2013). "Sudden infant death syndrome: review for the obstetric care provider". American Journal of Perinatology. 30 (9): 703–714. doi:10.1055/s-0032-1331035. PMID 23292938. S2CID 25034518.
- ^ Phillips DP, Brewer KM, Wadensweiler P (March 2011). "Alcohol as a risk factor for sudden infant death syndrome (SIDS)". Addiction. 106 (3): 516–525. doi:10.1111/j.1360-0443.2010.03199.x. PMID 21059188. Archived from the original on 6 September 2017. Retrieved 6 September 2017.
- ^ O'Leary CM, Jacoby PJ, Bartu A, D'Antoine H, Bower C (March 2013). "Maternal alcohol use and sudden infant death syndrome and infant mortality excluding SIDS". Pediatrics. 131 (3): e770–e778. doi:10.1542/peds.2012-1907. PMID 23439895. S2CID 2523083.
- ^ a b c d e Friedman HS (26 August 2011). The Oxford Handbook of Health Psychology. Oxford University Press, USA. pp. 699–. ISBN 978-0-19-534281-9.
- ^ "No level of alcohol consumption is safe for our health". www.who.int. Retrieved 13 October 2023.
- ^ Peacock A, Leung J, Larney S, Colledge S, Hickman M, Rehm J, et al. (October 2018). "Global statistics on alcohol, tobacco and illicit drug use: 2017 status report". Addiction. 113 (10): 1905–1926. doi:10.1111/add.14234. hdl:11343/283940. PMID 29749059.
- ^ Reimold D (29 May 2012). "College Word of the Year Contest contenders: Drunkorexia, shmacked and FOMO". The Washington Post. Retrieved 16 November 2012.
- ^ a b Alcohol-Related Psychosis at eMedicine
- ^ Tien AY, Anthony JC (August 1990). "Epidemiological analysis of alcohol and drug use as risk factors for psychotic experiences". The Journal of Nervous and Mental Disease. 178 (8): 473–480. doi:10.1097/00005053-199017880-00001. PMID 2380692.
- ^ Cargiulo T (March 2007). "Understanding the health impact of alcohol dependence". American Journal of Health-System Pharmacy. 64 (5 Suppl 3): S5-11. doi:10.2146/ajhp060647. PMID 17322182.
- ^ Schuckit MA (November 1983). "Alcoholism and other psychiatric disorders". Hospital & Community Psychiatry. 34 (11): 1022–1027. doi:10.1176/ps.34.11.1022. PMID 6642446.
- ^ Monnot, M., Nixon, S., Lovallo, W., & Ross, E. (2001). Altered emotional perception in alcoholics: Deficits in affective prosody comprehension. [Article]. Alcoholism: Clinical and Experimental Research, 25(3), 362–369.
- ^ Taieb O, Corcos M, Loas G, Speranza M, Guilbaud O, Perez-Diaz F, et al. (May 2002). "[Alexithymia and alcohol dependence]". Annales de Médecine Interne. 153 (3 Suppl): 1S51–1S60. PMID 12218885.
- ^ Uekermann J, Daum I (May 2008). "Social cognition in alcoholism: a link to prefrontal cortex dysfunction?". Addiction. 103 (5). Wiley-Blackwell: 726–735. doi:10.1111/j.1360-0443.2008.02157.x. PMID 18412750.
- ^ a b Hendler RA, Ramchandani VA, Gilman J, Hommer DW (2013). "Stimulant and sedative effects of alcohol". Current Topics in Behavioral Neurosciences. 13: 489–509. doi:10.1007/7854_2011_135. ISBN 978-3-642-28719-0. PMID 21560041.
- ^ a b c Dumain T. Pathak N (ed.). "Peptic Ulcer Disease (Stomach Ulcers) Cause, Symptoms, Treatments". Webmd.com. Retrieved 27 April 2013.
- ^ Patel S, Behara R, Swanson GR, Forsyth CB, Voigt RM, Keshavarzian A (October 2015). "Alcohol and the Intestine". Biomolecules. 5 (4): 2573–88. doi:10.3390/biom5042573. PMC 4693248. PMID 26501334.
- ^ Stephens R, Ling J, Heffernan TM, Heather N, Jones K (23 January 2008). "A review of the literature on the cognitive effects of alcohol hangover". Alcohol and Alcoholism. 43 (2): 163–170. doi:10.1093/alcalc/agm160. PMID 18238851.
- ^ "Hangxiety: why alcohol can leave you feeling anxious". Queensland Health. Queensland Health. The State of Queensland. 26 July 2023. Retrieved 2 October 2024.
- ^ a b Pittler MH, Verster JC, Ernst E (December 2005). "Interventions for preventing or treating alcohol hangover: systematic review of randomised controlled trials". BMJ. 331 (7531): 1515–1518. doi:10.1136/bmj.331.7531.1515. PMC 1322250. PMID 16373736.
- ^ "A get-sober pill?". Science News (Paper magazine). 202 (9): 4. 19 November 2022.
- ^ Verster JC, Stephens R, Penning R, Rohsenow D, McGeary J, Levy D, et al. (Alcohol Hangover Research Group) (June 2010). "The alcohol hangover research group consensus statement on best practice in alcohol hangover research". Current Drug Abuse Reviews. 3 (2): 116–126. doi:10.2174/1874473711003020116. PMC 3827719. PMID 20712593.
- ^ Jain A, Yelamanchili VS, Brown KN, Goel A (2024). "Holiday Heart Syndrome". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 30725870. Retrieved 15 February 2024.
- ^ "Holiday heart syndrome – definition". Biology-Online.org.
- ^ Rosenthal L, Stokken GT, Smith RH, Daubert JP, Weiss HS, Budzikowski AS (17 October 2021). Talavera F, Compton SJ, Dizon JM (eds.). "Holiday Heart Syndrome: Background, Pathophysiology, Epidemiology". Medscape.
- ^ Ettinger PO, Wu CF, De La Cruz C, Weisse AB, Ahmed SS, Regan TJ (May 1978). "Arrhythmias and the "Holiday Heart": alcohol-associated cardiac rhythm disorders". American Heart Journal. 95 (5): 555–562. doi:10.1016/0002-8703(78)90296-x. PMID 636996.
- ^ Tonelo D, Providência R, Gonçalves L (August 2013). "Holiday heart syndrome revisited after 34 years". Arquivos Brasileiros de Cardiologia. 101 (2): 183–189. doi:10.5935/abc.20130153. PMC 3998158. PMID 24030078.
- ^ Brown KN, Yelamanchili VS, Goel A (2022). "Holiday Heart Syndrome". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 30725870. Retrieved 26 August 2022.
- ^ Money KE, Myles WS (February 1974). "Heavy water nystagmus and effects of alcohol". Nature. 247 (5440): 404–405. Bibcode:1974Natur.247..404M. doi:10.1038/247404a0. PMID 4544739. S2CID 4166559.
- ^ a b Brooks PJ, Enoch MA, Goldman D, Li TK, Yokoyama A (March 2009). "The alcohol flushing response: an unrecognized risk factor for esophageal cancer from alcohol consumption". PLOS Medicine. 6 (3): e50. doi:10.1371/journal.pmed.1000050. PMC 2659709. PMID 19320537.
- ^ McMurran M (3 October 2012). Alcohol-Related Violence: Prevention and Treatment. John Wiley & Sons. p. 37. ISBN 978-1-118-41106-3.
- ^ Adams KE, Rans TS (December 2013). "Adverse reactions to alcohol and alcoholic beverages". Annals of Allergy, Asthma & Immunology. 111 (6): 439–45. doi:10.1016/j.anai.2013.09.016. PMID 24267355.
- ^ "Alcohol Flush Signals Increased Cancer Risk among East Asians". News Release. National Institutes of Health (NIH). 23 March 2009. Archived from the original on 16 February 2012.
- ^ Lee CH, Lee JM, Wu DC, Goan YG, Chou SH, Wu IC, et al. (March 2008). "Carcinogenetic impact of ADH1B and ALDH2 genes on squamous cell carcinoma risk of the esophagus with regard to the consumption of alcohol, tobacco and betel quid". International Journal of Cancer. 122 (6): 1347–1356. doi:10.1002/ijc.23264. PMID 18033686.
- ^ "Unravelling the commercial determinants of health". The Lancet (Editorial). 401 (10383): 1131. 23 March 2023. doi:10.1016/S0140-6736(23)00590-1. PMID 36966781.
- ^ "Just four industries cause 2.7 million deaths in the European Region every year". World Health Organization. 12 June 2024. Retrieved 12 June 2024.
Four corporate products – tobacco, ultra-processed foods, fossil fuels and alcohol – cause 19 million deaths per year globally, or 34% of all deaths.
- ^ Bawden A, Campbell D (12 June 2024). "Tobacco, alcohol, processed foods and fossil fuels 'kill 2.7m a year in Europe'". The Guardian. Retrieved 12 June 2024.
- ^ a b Mathurin P, Deltenre P (May 2009). "Effect of binge drinking on the liver: an alarming public health issue?". Gut. 58 (5): 613–17. doi:10.1136/gut.2007.145573. PMID 19174416. S2CID 43370272.
- ^ Mekonen T, Chan GC, Connor J, Hall W, Hides L, Leung J (October 2021). "Treatment rates for alcohol use disorders: a systematic review and meta-analysis". Addiction. 116 (10): 2617–2634. doi:10.1111/add.15357. PMID 33245581. S2CID 227180779.
- ^ a b c d e f g h i j k l m n o Butcher JN, Hooley JM, Mineka SM (25 June 2013). Abnormal Psychology. Pearson Education. p. 370. ISBN 978-0-205-97175-6.
- ^ Bakalar N (27 August 2018). "How Much Alcohol Is Safe to Drink? None, Say These Researchers". The New York Times. Retrieved 17 September 2018.
- ^ Kilian C, Manthey J, Carr S, Hanschmidt F, Rehm J, Speerforck S, et al. (May 2021). "Stigmatization of people with alcohol use disorders: An updated systematic review of population studies". Alcoholism: Clinical and Experimental Research. 45 (5): 899–911. doi:10.1111/acer.14598. PMID 33970504.
- ^ Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC (2011). "The stigma of alcohol dependence compared with other mental disorders: a review of population studies". Alcohol and Alcoholism. 46 (2): 105–112. doi:10.1093/alcalc/agq089. PMID 21169612.
- ^ Tomlinson A (26 June 2018). "Tips and Tricks on How to Cut Down on the Booze". The West Australian. Seven West Media (WA). Retrieved 22 March 2019.
- ^ "Alcohol". British Liver Trust. Archived from the original on 11 July 2019. Retrieved 22 March 2019.
- ^ "What to Know About Dry Drunk Syndrome".
- ^ Brook DW, Spitz HI (23 September 2002). The Group Therapy of Substance Abuse. CRC Press. p. 73. ISBN 978-0-7890-1782-6.
- ^ Benton SA (2009). Understanding the High-Functioning Alcoholic – Professional Views and Personal Insights. Greenwood Publishing Group. ISBN 978-0-313-35280-5.
- ^ Brody J (4 May 2009). "High Functioning, but Still Alcoholics". The New York Times. Retrieved 18 February 2012.
- ^ "What is a High Functioning Alcoholic? | Definition & Signs". Alcohol.org. Retrieved 29 January 2021.
- ^ Szlemko WJ, Wood JW, Thurman PJ (October 2006). "Native Americans and alcohol: past, present, and future". The Journal of General Psychology. 133 (4). Heldref Publications: 435–451. doi:10.3200/GENP.133.4.435-451. PMID 17128961. S2CID 43082343.
- ^ a b Arts NJ, Walvoort SJ, Kessels RP (27 November 2017). "Korsakoff's syndrome: a critical review". Neuropsychiatric Disease and Treatment. 13: 2875–2890. doi:10.2147/NDT.S130078. PMC 5708199. PMID 29225466.
- ^ Ridley NJ, Draper B, Withall A (25 January 2013). "Alcohol-related dementia: an update of the evidence". Alzheimer's Research & Therapy. 5 (1): 3. doi:10.1186/alzrt157. PMC 3580328. PMID 23347747.
- ^ synd/2922 at Who Named It?
- ^ E. Marchiafava, A. Bignami. Sopra un'alterazione del corpo calloso osservata da sogetti alcoolisti. Rivista di patologia nervosa e mentale, 1903, 8 (12): 544–549.
- ^ Raina, Sujeet & M Mahesh, D & Mahajan, J & S Kaushal, S & Gupta, D & Dhiman, Dalip. (2008). MarchiafavaBignami Disease. The Journal of the Association of Physicians of India. 56. 633-5.
- ^ Bruha R, Dvorak K, Petrtyl J (March 2012). "Alcoholic liver disease". World Journal of Hepatology. 4 (3): 81–90. doi:10.4254/wjh.v4.i3.81. PMC 3321494. PMID 22489260.
- ^ 15th Report on Carcinogens. National Toxicology Program (NTP) (Report). doi:10.22427/ntp-other-1003. S2CID 245412518.
- ^ Hashibe M, Brennan P, Chuang SC, Boccia S, Castellsague X, Chen C, et al. (February 2009). "Interaction between tobacco and alcohol use and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium". Cancer Epidemiology, Biomarkers & Prevention. 18 (2): 541–550. doi:10.1158/1055-9965.EPI-08-0347. PMC 3051410. PMID 19190158.
- ^ Petticrew M, Maani Hessari N, Knai C, Weiderpass E (March 2018). "How alcohol industry organisations mislead the public about alcohol and cancer" (PDF). Drug and Alcohol Review. 37 (3): 293–303. doi:10.1111/dar.12596. PMID 28881410.
- ^ a b Piano MR (2017). "Alcohol's Effects on the Cardiovascular System". Alcohol Research. 38 (2): 219–241. PMC 5513687. PMID 28988575.
- ^ Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G (March 2010). "Alcohol consumption and mortality in patients with cardiovascular disease: a meta-analysis". Journal of the American College of Cardiology. 55 (13): 1339–1347. doi:10.1016/j.jacc.2010.01.006. PMID 20338495.
- ^ "Alcohol and Heart Health". American Heart Association. 15 August 2014.
- ^ Arora M, ElSayed A, Beger B, Naidoo P, Shilton T, Jain N, et al. (2022). "The Impact of Alcohol Consumption on Cardiovascular Health: Myths and Measures" (PDF). Global Heart. 17 (1): 45. doi:10.5334/gh.1132. PMC 9306675. PMID 36051324.
- ^ a b Salamon M (May 2022). "Want a healthier heart? Seriously consider skipping the drinks". Harvard Health.
- ^ Piano MR (May 2002). "Alcoholic cardiomyopathy: incidence, clinical characteristics, and pathophysiology". Chest. 121 (5): 1638–1650. doi:10.1378/chest.121.5.1638. PMC 1923411. PMID 12006456.
- ^ a b Bellé M, Sartori Sd, Rossi AG (January 2007). "Alcoholism: effects on the cochleo-vestibular apparatus". Brazilian Journal of Otorhinolaryngology. 73 (1): 110–116. doi:10.1016/s1808-8694(15)31132-0. PMC 9443585. PMID 17505609.
- ^ Upile T, Sipaul F, Jerjes W, Singh S, Nouraei SA, El Maaytah M, et al. (September 2007). "The acute effects of alcohol on auditory thresholds". BMC Ear, Nose and Throat Disorders. 7: 4. doi:10.1186/1472-6815-7-4. PMC 2031886. PMID 17877829.
- ^ Qian P, Zhao Z, Liu S, Xin J, Liu Y, Hao Y, et al. (2023). "Alcohol as a risk factor for hearing loss: A systematic review and meta-analysis". PLOS ONE. 18 (1): e0280641. Bibcode:2023PLoSO..1880641Q. doi:10.1371/journal.pone.0280641. PMC 9858841. PMID 36662896.
- ^ Ashworth M, Gerada C (August 1997). "ABC of mental health. Addiction and dependence – II: Alcohol". BMJ. 315 (7104): 358–360. doi:10.1136/bmj.315.7104.358. PMC 2127236. PMID 9270461.
- ^ Fisher GL, Roget NA, eds. (2009). "Withdrawal: Alcohol". Encyclopedia of substance abuse prevention, treatment, & recovery. Los Angeles: SAGE. p. 1005. ISBN 978-1-4522-6601-5. Archived from the original on 22 December 2015.
- ^ McClure EA, Gipson CD, Malcolm RJ, Kalivas PW, Gray KM (2014). "Potential role of N-acetylcysteine in the management of substance use disorders". CNS Drugs. 28 (2): 95–106. doi:10.1007/s40263-014-0142-x. PMC 4009342. PMID 24442756.
- ^ Qu L, Ma XP, Simayi A, Wang XL, Xu GP (May 2024). "Comparative efficacy of various pharmacologic treatments for alcohol withdrawal syndrome: a systematic review and network meta-analysis". International Clinical Psychopharmacology. 39 (3): 148–162. doi:10.1097/YIC.0000000000000526. PMID 38170803.
- ^ Gillman M.A, Lichtigfeld, F.J. 2004 Enlarged double-blind randomised trial of benzodiazepines against psychotropic analgesic nitrous oxide for alcohol withdrawal, Addictive Behaviors, Volume 29, Issue 6, Pages 1183–1187
- ^ Ebrahimpour-Koujan S, Saneei P, Larijani B, Esmaillzadeh A (2020). "Consumption of sugar sweetened beverages and dietary fructose in relation to risk of gout and hyperuricemia: a systematic review and meta-analysis". Critical Reviews in Food Science and Nutrition. 60 (1): 1–10. doi:10.1080/10408398.2018.1503155. PMID 30277800. S2CID 52909165.
- ^ Singh JA, Reddy SG, Kundukulam J (March 2011). "Risk factors for gout and prevention: a systematic review of the literature". Current Opinion in Rheumatology. 23 (2): 192–202. doi:10.1097/BOR.0b013e3283438e13. PMC 4104583. PMID 21285714.
- ^ Roddy E, Mallen CD, Doherty M (October 2013). "Gout". BMJ. 347 (oct01 3): f5648. doi:10.1136/bmj.f5648. PMID 24473446. S2CID 220212466.
- ^ Allison MG, McCurdy MT (May 2014). "Alcoholic metabolic emergencies". Emergency Medicine Clinics of North America. 32 (2): 293–301. doi:10.1016/j.emc.2013.12.002. PMID 24766933.
- ^ Howard RD, Bokhari SR (January 2019). Alcoholic Ketoacidosis (AKA). PMID 28613672.
- ^ a b McGuire LC, Cruickshank AM, Munro PT (June 2006). "Alcoholic ketoacidosis". Emergency Medicine Journal. 23 (6): 417–420. doi:10.1136/emj.2004.017590. PMC 2564331. PMID 16714496.
- ^ Palzes VA, Parthasarathy S, Chi FW, Kline-Simon AH, Lu Y, Weisner C, et al. (December 2020). "Associations Between Psychiatric Disorders and Alcohol Consumption Levels in an Adult Primary Care Population". Alcoholism: Clinical and Experimental Research. 44 (12): 2536–2544. doi:10.1111/acer.14477. PMC 7756330. PMID 33151592.
- ^ Jané-Llopis E, Matytsina I (November 2006). "Mental health and alcohol, drugs and tobacco: a review of the comorbidity between mental disorders and the use of alcohol, tobacco and illicit drugs". Drug and Alcohol Review. 25 (6): 515–536. doi:10.1080/09595230600944461. PMID 17132571.
- ^ Shi X, Li M, Yao J, Li MD, Yang Z (July 2024). "Alcohol drinking, DNA methylation and psychiatric disorders: A multi-omics Mendelian randomization study to investigate causal pathways". Addiction. 119 (7): 1226–1237. doi:10.1111/add.16465. PMID 38523595.
- ^ Georgiadou SP, Manoulakas E, Makaritsis KP, Dalekos GN (May 2018). "A chronic alcoholic man with high fever, neck rigidity and loss of consciousness: remember the Austrian syndrome a commonly unrecognised invasive pneumococcus triad". BMJ Case Reports. 2018: bcr–2018–225010. doi:10.1136/bcr-2018-225010. PMC 5976089. PMID 29848535.
- ^ Starek-Świechowicz B, Budziszewska B, Starek A (February 2023). "Alcohol and breast cancer". Pharmacological Reports. 75 (1): 69–84. doi:10.1007/s43440-022-00426-4. PMC 9889462. PMID 36310188.
- ^ "Shouldn't we know this already? The link between alcohol and breast cancer". www.who.int.
- ^ "Alcohol". Drugs and Lactation Database (LactMed) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development. September 2024. PMID 30000529.
- ^ "Neonatal abstinence Syndrome". MedlinePlus. US Library of Medicine. 2017. Retrieved 27 July 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Ghazanfarpour M, Najafi MN, Roozbeh N, Mashhadi ME, Keramat-Roudi A, Mégarbane B, et al. (June 2019). "Therapeutic approaches for neonatal abstinence syndrome: a systematic review of randomized clinical trials". Daru: Journal of Faculty of Pharmacy, Tehran University of Medical Sciences. 27 (1): 423–431. doi:10.1007/s40199-019-00266-3. PMC 6593026. PMID 31093953.
- ^ Ko JY, Wolicki S, Barfield WD, Patrick SW, Broussard CS, Yonkers KA, et al. (2017). "CDC Grand Rounds: Public Health Strategies to Prevent Neonatal Abstinence Syndrome". MMWR. Morbidity and Mortality Weekly Report. 66 (9): 242–245. doi:10.15585/mmwr.mm6609a2. PMC 5687191. PMID 28278146.
- ^ Rehm J, Samokhvalov AV, Neuman MG, Room R, Parry C, Lönnroth K, et al. (December 2009). "The association between alcohol use, alcohol use disorders and tuberculosis (TB). A systematic review". BMC Public Health. 9: 450. doi:10.1186/1471-2458-9-450. PMC 2796667. PMID 19961618.
- ^ Lönnroth K, Williams BG, Stadlin S, Jaramillo E, Dye C (August 2008). "Alcohol use as a risk factor for tuberculosis - a systematic review". BMC Public Health. 8: 289. doi:10.1186/1471-2458-8-289. PMC 2533327. PMID 18702821.
- ^ Sorkin T, Sheppard MN (September 2017). "Sudden unexplained death in alcohol misuse (SUDAM) patients have different characteristics to those who died from sudden arrhythmic death syndrome (SADS)". Forensic Science, Medicine, and Pathology. 13 (3): 278–283. doi:10.1007/s12024-017-9877-2. PMC 5554285. PMID 28668989.
- ^ Sveinsson O, Andersson T, Mattsson P, Carlsson S, Tomson T (January 2020). "Clinical risk factors in SUDEP: A nationwide population-based case-control study". Neurology. 94 (4): e419–e429. doi:10.1212/WNL.0000000000008741. PMC 7079690. PMID 31831600.
- ^ Ricci E, Al Beitawi S, Cipriani S, Candiani M, Chiaffarino F, Viganò P, et al. (January 2017). "Semen quality and alcohol intake: a systematic review and meta-analysis". Reproductive Biomedicine Online. 34 (1): 38–47. doi:10.1016/j.rbmo.2016.09.012. PMID 28029592.
- ^ "What Causes Insomnia?". NHLBI. 13 December 2011. Archived from the original on 28 July 2016. Retrieved 9 August 2016.
- ^ "Restless Legs Syndrome Fact Sheet | National Institute of Neurological Disorders and Stroke". Ninds.nih.gov. Archived from the original on 28 July 2017. Retrieved 7 July 2019.
- ^ "Sleep Apnea - Causes and Risk Factors | NHLBI, NIH". 24 March 2022. Archived from the original on 6 February 2024. Retrieved 6 February 2024.
- ^ Klop B, do Rego AT, Cabezas MC (August 2013). "Alcohol and plasma triglycerides". Current Opinion in Lipidology. 24 (4): 321–326. doi:10.1097/MOL.0b013e3283606845. PMID 23511381.
- ^ "Pancreatitis". A.D.A.M., Inc. Archived from the original on 30 December 2012. Retrieved 5 January 2013.
- ^ Apte MV, Pirola RC, Wilson JS (June 2009). "Pancreas: alcoholic pancreatitis—it's the alcohol, stupid". Nature Reviews. Gastroenterology & Hepatology. 6 (6): 321–2. doi:10.1038/nrgastro.2009.84. PMID 19494819. S2CID 6580794.
- Lay summary in: Apte MV, Pirola RC, Wilson JS. "Pancreas: Alcoholic Pancreatitis—It's the Alcohol, Stupid". Medscape Today.
- ^ Yadav D, Hawes RH, Brand RE, Anderson MA, Money ME, Banks PA, et al. (June 2009). "Alcohol consumption, cigarette smoking, and the risk of recurrent acute and chronic pancreatitis". Archives of Internal Medicine. 169 (11): 1035–45. doi:10.1001/archinternmed.2009.125. PMC 6785300. PMID 19506173.
- ^ "Pancreatitis Explained". Better Health Channel. State Government of Victoria. 2011. Archived from the original on 13 May 2010.
- ^ Johnson CD, Hosking S (November 1991). "National statistics for diet, alcohol consumption, and chronic pancreatitis in England and Wales, 1960–88". Gut. 32 (11): 1401–5. doi:10.1136/gut.32.11.1401. PMC 1379177. PMID 1752477.
- ^ Porphyria Cutanea Tarda at eMedicine
- ^ Hart MG, Hooper G (July 2005). "Clinical associations of Dupuytren's disease". Postgraduate Medical Journal. 81 (957): 425–428. doi:10.1136/pgmj.2004.027425. PMC 1743313. PMID 15998816.
- ^ Burge P, Hoy G, Regan P, Milne R (March 1997). "Smoking, alcohol and the risk of Dupuytren's contracture". The Journal of Bone and Joint Surgery. British Volume. 79 (2): 206–210. doi:10.1302/0301-620x.79b2.6990. PMID 9119843.
- ^ Cardet JC, White AA, Barrett NA, Feldweg AM, Wickner PG, Savage J, et al. (2014). "Alcohol-induced respiratory symptoms are common in patients with aspirin exacerbated respiratory disease". The Journal of Allergy and Clinical Immunology. In Practice. 2 (2): 208–13. doi:10.1016/j.jaip.2013.12.003. PMC 4018190. PMID 24607050.
- ^ a b Nutt DJ, King LA, Phillips LD (November 2010). "Drug harms in the UK: a multicriteria decision analysis". Lancet. 376 (9752): 1558–1565. CiteSeerX 10.1.1.690.1283. doi:10.1016/S0140-6736(10)61462-6. PMID 21036393. S2CID 5667719.
- ^ a b Nutt D, King LA, Saulsbury W, Blakemore C (March 2007). "Development of a rational scale to assess the harm of drugs of potential misuse". Lancet. 369 (9566): 1047–1053. doi:10.1016/s0140-6736(07)60464-4. PMID 17382831. S2CID 5903121.
- ^ a b c d e f g h Sunga HE (2016). "Alcohol and Crime". The Blackwell Encyclopedia of Sociology. American Cancer Society. pp. 1–2. doi:10.1002/9781405165518.wbeosa039.pub2. ISBN 978-1-4051-6551-8.
- ^ Trevor B, Katy H (1 April 2005). Understanding Drugs, Alcohol And Crime. McGraw-Hill Education (UK). p. 6. ISBN 978-0-335-21257-6.
- ^ "Drunk Driving Statistics in the US and Across the World". Law Office of Douglas Herring. 13 November 2017. Archived from the original on 22 September 2019. Retrieved 22 September 2019.
- ^ "Drunk Driving Increasing Concern Worldwide". Voice of America. Retrieved 22 September 2019.
- ^ Sweedler BM, Stewart K (2009). "Worldwide trends in alcohol and drug impaired driving". In Verster JC, Pandi-Perumal SR, Ramaekers JG, de Gier JJ (eds.). Drugs, Driving and Traffic Safety. Birkhäuser Basel. pp. 23–41. doi:10.1007/978-3-7643-9923-8_2. ISBN 978-3-7643-9923-8.
- ^ a b c d Clinard M, Meier R (14 February 2007). Sociology of Deviant Behavior. Cengage Learning. p. 273. ISBN 978-0-495-09335-0.
- ^ a b McMurran M (3 October 2012). Alcohol-Related Violence: Prevention and Treatment. John Wiley & Sons. pp. 337–338. ISBN 978-1-118-41106-3.
- ^ a b c McMurran M (3 October 2012). Alcohol-Related Violence: Prevention and Treatment. John Wiley & Sons. p. 37. ISBN 978-1-118-41106-3.
- ^ "WHO | Governments confront drunken violence". WHO. Archived from the original on 4 May 2014. Retrieved 22 September 2019.
- ^ a b "Global status report on alcohol and health" (PDF). World Health Organization. 2011.
- ^ Smith R (16 March 2010). "'Passive drinking' is blighting the nation, Sir Liam Donaldson warns". The Daily Telegraph. Archived from the original on 20 March 2009. Retrieved 30 May 2010.
- ^ Hingson R, Winter M (2003). "Epidemiology and consequences of drinking and driving". Alcohol Research & Health. 27 (1): 63–78. PMC 6676697. PMID 15301401.
- ^ Naranjo CA, Bremner KE (January 1993). "Behavioural correlates of alcohol intoxication". Addiction. 88 (1): 25–35. doi:10.1111/j.1360-0443.1993.tb02761.x. PMID 8448514.
- ^ Driving Under the Influence: A Report to Congress on Alcohol Limits. U.S. Department of Transportation, National Highway Traffic Safety Administration. 1992. pp. 1–.
- ^ "Legislative History of .08 per se Laws – NHTSA". NHTSA. National Highway Traffic Safety Administration. July 2001. Retrieved 21 July 2017.
- ^ Nelson B. "Nevada's Driving Under the Influence (DUI) laws". NVPAC. Advisory Council for Prosecuting Attorneys. Archived from the original on 22 April 2017. Retrieved 3 July 2017.
- ^ Bothorn JB, Schwender H, Graw M, Kienbaum P, Hartung B (July 2022). "Cycling under the influence of alcohol-criminal offenses in a German metropolis". International Journal of Legal Medicine. 136 (4): 1121–1132. doi:10.1007/s00414-022-02828-8. PMC 9170663. PMID 35474490.
- ^ Sethi M, Heyer JH, Wall S, DiMaggio C, Shinseki M, Slaughter D, et al. (June 2016). "Alcohol use by urban bicyclists is associated with more severe injury, greater hospital resource use, and higher mortality". Alcohol. 53: 1–7. doi:10.1016/j.alcohol.2016.03.005. PMC 5248656. PMID 27286931.
- ^ a b Hall JA, Moore CB (July 2008). "Drug facilitated sexual assault—a review". Journal of Forensic and Legal Medicine. 15 (5): 291–7. doi:10.1016/j.jflm.2007.12.005. PMID 18511003.
- ^ Davis KC, Schraufnagel TJ, George WH, Norris J (September 2008). "The use of alcohol and condoms during sexual assault". American Journal of Men's Health. 2 (3): 281–290. doi:10.1177/1557988308320008. PMC 4617377. PMID 19477791.
- ^ Price S (2007). Mental Health in Pregnancy and Childbirth. Elsevier Health Sciences. pp. 151–152. ISBN 978-0-443-10317-9. Retrieved 15 February 2013.
- ^ ElSohly MA, Salamone SJ (1999). "Prevalence of drugs used in cases of alleged sexual assault". Journal of Analytical Toxicology. 23 (3): 141–146. doi:10.1093/jat/23.3.141. PMID 10369321.
- ^ a b "Alcohol Is Most Common 'Date Rape' Drug". Medicalnewstoday.com. Archived from the original on 17 October 2007. Retrieved 1 June 2011.
- ^ Schwartz RH, Milteer R, LeBeau MA (June 2000). "Drug-facilitated sexual assault ('date rape')". Southern Medical Journal. 93 (6): 558–61. doi:10.1097/00007611-200093060-00002. PMID 10881768.
- ^ a b Holstege CP, Saathoff GB, Neer TM, Furbee RB, eds. (25 October 2010). Criminal poisoning: clinical and forensic perspectives. Sudbury, Mass.: Jones and Bartlett Publishers. pp. 232. ISBN 978-0-7637-4463-2.
- ^ Lyman MD (2006). Practical drug enforcement (3rd ed.). Boca Raton, Fla.: CRC. p. 70. ISBN 0-8493-9808-8.
- ^ Thompson KM (January 2021). "Beyond roofies: Drug- and alcohol-facilitated sexual assault". JAAPA. 34 (1): 45–49. doi:10.1097/01.JAA.0000723940.92815.0b. PMID 33332834.
- ^ Beynon CM, McVeigh C, McVeigh J, Leavey C, Bellis MA (July 2008). "The involvement of drugs and alcohol in drug-facilitated sexual assault: a systematic review of the evidence". Trauma, Violence & Abuse. 9 (3): 178–88. doi:10.1177/1524838008320221. PMID 18541699. S2CID 27520472.
- ^ "Date Rape". Survive.org.uk. 20 March 2000. Retrieved 1 June 2011.
- ^ Chersich MF, Rees HV (January 2010). "Causal links between binge drinking patterns, unsafe sex and HIV in South Africa: its time to intervene". International Journal of STD & AIDS. 21 (1): 2–7. doi:10.1258/ijsa.2000.009432. PMID 20029060. S2CID 3100905.
- ^ "Consumption of alcohol/energy drink mixes linked with casual, risky sex". ScienceDaily.
- ^ a b Ball NJ, Miller KE, Quigley BM, Eliseo-Arras RK (April 2021). "Alcohol Mixed With Energy Drinks and Sexually Related Causes of Conflict in the Barroom". Journal of Interpersonal Violence. 36 (7–8): 3353–3373. doi:10.1177/0886260518774298. PMID 29779427. S2CID 29150434.
- ^ Hatch J (21 April 2017). "Inside The Online Community Of Men Who Preach Removing Condoms Without Consent". Huffington Post. Retrieved 23 April 2017.
- ^ Chesser B, Zahra A (22 May 2019). "Stealthing: a criminal offence?". Current Issues in Criminal Justice. 31 (2). Sydney Law School: 217–235. doi:10.1080/10345329.2019.1604474. S2CID 182850828. Retrieved 18 February 2021.
- ^ Brodsky A (2017). "'Rape-Adjacent': Imagining Legal Responses to Nonconsensual Condom Removal". Columbia Journal of Gender and Law. 32 (2). SSRN 2954726.
- ^ Michael N (27 April 2017). "Some call it 'stealthing,' others call it sexual assault". CNN.
- ^ Davis KC, Danube CL, Neilson EC, Stappenbeck CA, Norris J, George WH, et al. (January 2016). "Distal and Proximal Influences on Men's Intentions to Resist Condoms: Alcohol, Sexual Aggression History, Impulsivity, and Social-Cognitive Factors". AIDS and Behavior. 20 (Suppl 1): S147–S157. doi:10.1007/s10461-015-1132-9. PMC 4706816. PMID 26156881.
- ^ Davis KC (October 2010). "The influence of alcohol expectancies and intoxication on men's aggressive unprotected sexual intentions". Experimental and Clinical Psychopharmacology. 18 (5): 418–428. doi:10.1037/a0020510. PMC 3000798. PMID 20939645.
- ^ "Njemačke žene nisu silovali samo sovjetski vojnici" [German women were not only raped by Soviet soldiers]. Deutsche Welle (in Croatian). Retrieved 2 July 2022.
- ^ "Rule 93. Rape and other forms of sexual violence are prohibited". International Humanitarian Law (IHL) Databases. International Committee of the Red Cross (ICRC).
- ^ "England gets a taste for Buckfast, the fortified wine that's linked to crime". The Daily Telegraph. 17 July 2017.
- ^ "Alcohol-Related Crimes: Statistics and Facts". Alcohol Rehab Guide. Retrieved 3 September 2019.
- ^ "Alcohol statistics". Alcohol Change UK. Retrieved 22 September 2019.
- ^ Naimi TS, Xuan Z, Cooper SE, Coleman SM, Hadland SE, Swahn MH, et al. (December 2016). "Alcohol Involvement in Homicide Victimization in the United States". Alcoholism: Clinical and Experimental Research. 40 (12): 2614–2621. doi:10.1111/acer.13230. PMC 5134733. PMID 27676334.
- ^ Dingwall G (23 July 2013). Alcohol and Crime. Routledge. pp. 160–161. ISBN 978-1-134-02970-9.
- ^ "Application to Include Fomepizole on the WHO Model List of Essential Medicines" (PDF). November 2012. p. 10.
- ^ a b Vale A (2007). "Methanol". Medicine. 35 (12): 633–4. doi:10.1016/j.mpmed.2007.09.014.
- ^ "Methanol Poisoning Overview". Antizol. Archived from the original on 5 October 2011. Retrieved 11 October 2011. dead link
- ^ "Methanol (CASRN 67–56–1)". Integrated Risk Information System (IRIS). U.S. Environmental Protection Agency.
- ^ Standridge JB, Zylstra RG, Adams SM (July 2004). "Alcohol consumption: an overview of benefits and risks". Southern Medical Journal. 97 (7): 664–672. doi:10.1097/00007611-200407000-00012. PMID 15301124. S2CID 26801239.
- ^ Kuntsche E, Rehm J, Gmel G (July 2004). "Characteristics of binge drinkers in Europe". Social Science & Medicine. 59 (1): 113–127. doi:10.1016/j.socscimed.2003.10.009. PMID 15087148.
- ^ Clark DB, Bukstein O, Cornelius J (2002). "Alcohol use disorders in adolescents: epidemiology, diagnosis, psychosocial interventions, and pharmacological treatment". Paediatric Drugs. 4 (8): 493–502. doi:10.2165/00128072-200204080-00002. PMID 12126453. S2CID 30900197.
- ^ Floyd RL, O'Connor MJ, Sokol RJ, Bertrand J, Cordero JF (November 2005). "Recognition and prevention of fetal alcohol syndrome". Obstetrics and Gynecology. 106 (5 Pt 1): 1059–1064. CiteSeerX 10.1.1.537.7292. doi:10.1097/01.AOG.0000181822.91205.6f. PMID 16260526.
- ^ Compare: Stolle M, Sack PM, Thomasius R (May 2009). "Binge drinking in childhood and adolescence: epidemiology, consequences, and interventions". Deutsches Ärzteblatt International. 106 (19): 323–328. doi:10.3238/arztebl.2009.0323. PMC 2689602. PMID 19547732.
Excessive episodic consumption of alcohol is usually referred to these days as 'binge drinking.'
- ^ Sher KJ, Grekin ER (2007). "Alcohol and affect regulation.". In Gross JJ (ed.). Handbook of Emotion Regulation. New York: Guilford Press. pp. 560–580. ISBN 978-1-60623-354-2.
- ^ Costa RM, Brody S (October 2013). "Immature psychological defense mechanisms are associated with greater personal importance of junk food, alcohol, and television". Psychiatry Research. 209 (3): 535–539. doi:10.1016/j.psychres.2013.06.035. PMID 23866675.
- ^ Konno Y, Okawara M, Hino A, Nagata T, Muramatsu K, Tateishi S, et al. (Project CORoNaWork) (December 2022). "Association of alcohol consumption and frequency with loneliness: A cross-sectional study among Japanese workers during the COVID-19 pandemic". Heliyon. 8 (12): e11933. Bibcode:2022Heliy...811933K. doi:10.1016/j.heliyon.2022.e11933. PMC 9729165. PMID 36510560.
- ^ Gutkind S, Gorfinkel LR, Hasin DS (January 2022). "Prospective effects of loneliness on frequency of alcohol and marijuana use". Addictive Behaviors. 124: 107115. doi:10.1016/j.addbeh.2021.107115. PMC 8511227. PMID 34543868.
- ^ Marano H. "The Dangers of Loneliness". Retrieved 10 December 2012.
- ^ Trub L, Doyle KM, Parker V, Starks TJ (2021). "Drunk Texting: When the Phone Becomes a Vehicle for Emotional Dysregulation and Problematic Alcohol Use". Substance Use & Misuse. 56 (12): 1815–1824. doi:10.1080/10826084.2021.1954027. PMID 34353214.
- ^ "Alcohol Policy Information Service". Archived from the original on 24 April 2011. Retrieved 19 April 2011.
- ^ van der Kruk S, Harrison NJ, Bartram A, Newton S, Miller C, Room R, et al. (October 2023). "Prevalence of parental supply of alcohol to minors: a systematic review". Health Promotion International. 38 (5). doi:10.1093/heapro/daad111. PMC 10533326. PMID 37758201.
- ^ Sharmin S, Kypri K, Khanam M, Wadolowski M, Bruno R, Mattick RP (March 2017). "Parental Supply of Alcohol in Childhood and Risky Drinking in Adolescence: Systematic Review and Meta-Analysis". International Journal of Environmental Research and Public Health. 14 (3): 287. doi:10.3390/ijerph14030287. PMC 5369123. PMID 28282955.
 This article incorporates text from this source, which is available under the CC BY 4.0 license.
This article incorporates text from this source, which is available under the CC BY 4.0 license.
- ^ Tael-Öeren M, Naughton F, Sutton S (September 2019). "The relationship between parental attitudes and children's alcohol use: a systematic review and meta-analysis" (PDF). Addiction. 114 (9): 1527–1546. doi:10.1111/add.14615. PMID 31185534.
- ^ Staff J, Maggs JL (January 2020). "Parents Allowing Drinking Is Associated With Adolescents' Heavy Alcohol Use". Alcoholism: Clinical and Experimental Research. 44 (1): 188–195. doi:10.1111/acer.14224. PMC 6980970. PMID 31750959.
- ^ a b Garcia C, Reiber SG, Massey AM (February 2013). "Sexual Hook-up Culture". Monitor on Psychology. Vol. 44, no. 2. American Psychological Association. p. 60. Retrieved 4 June 2013.
- ^ Fielder RL, Carey MP (October 2010). "Predictors and consequences of sexual "hookups" among college students: a short-term prospective study". Archives of Sexual Behavior. 39 (5): 1105–1119. doi:10.1007/s10508-008-9448-4. PMC 2933280. PMID 19130207.
- ^ Lewis MA, Granato H, Blayney JA, Lostutter TW, Kilmer JR (October 2012). "Predictors of hooking up sexual behaviors and emotional reactions among U.S. college students". Archives of Sexual Behavior. 41 (5): 1219–1229. doi:10.1007/s10508-011-9817-2. PMC 4397976. PMID 21796484.
- ^ Freitas D (2013). The End of Sex: How Hookup Culture is Leaving a Generation Unhappy, Sexually Unfulfilled, and Confused About Intimacy. New York: Basic Books. ISBN 978-0-465-00215-3.
- ^ Paul EL, McManus B, Hayes A (2000). "'Hookups': Characteristics and Correlates of College Students' Spontaneous and Anonymous Sexual Experiences". Journal of Sex Research. 37 (1): 76–88. doi:10.1080/00224490009552023.
- ^ Santelli JS, Brener ND, Lowry R, Bhatt A, Zabin LS (November 1998). "Multiple sexual partners among U.S. adolescents and young adults". Family Planning Perspectives. 30 (6): 271–275. doi:10.2307/2991502. JSTOR 2991502. PMID 9859017.
- ^ Halpern-Felsher BL, Millstein SG, Ellen JM (November 1996). "Relationship of alcohol use and risky sexual behavior: a review and analysis of findings". The Journal of Adolescent Health. 19 (5): 331–336. doi:10.1016/S1054-139X(96)00024-9. PMID 8934293.
- ^ Neilson EC, Marcantonio TL, Woerner J, Leone RM, Haikalis M, Davis KC (March 2024). "Alcohol intoxication, condom use rationale, and men's coercive condom use resistance: The role of past unintended partner pregnancy". Psychology of Addictive Behaviors. 38 (2): 173–184. doi:10.1037/adb0000956. PMC 10932814. PMID 37707467.
- ^ Davis KC, Masters NT, Eakins D, Danube CL, George WH, Norris J, et al. (January 2014). "Alcohol intoxication and condom use self-efficacy effects on women's condom use intentions". Addictive Behaviors. 39 (1): 153–158. doi:10.1016/j.addbeh.2013.09.019. PMC 3940263. PMID 24129265.
- ^ Rogow D, Horowitz S (1995). "Withdrawal: a review of the literature and an agenda for research". Studies in Family Planning. 26 (3): 140–153. doi:10.2307/2137833. JSTOR 2137833. PMID 7570764., which cites:
- Population Action International (1991). "A Guide to Methods of Birth Control." Briefing Paper No. 25, Washington, D. C.
- ^ Casey FE (20 March 2024). Talavera F, Barnes AD (eds.). "Coitus interruptus". Medscape.com. Archived from the original on 29 July 2019. Retrieved 24 July 2019.
- ^ a b Castles A, Adams EK, Melvin CL, Kelsch C, Boulton ML (April 1999). "Effects of smoking during pregnancy. Five meta-analyses". American Journal of Preventive Medicine. 16 (3): 208–215. doi:10.1016/S0749-3797(98)00089-0. PMID 10198660. S2CID 33535194.
- ^ a b Eisenberg L, Brown SH (1995). The best intentions: unintended pregnancy and the well-being of children and families. Washington, D.C.: National Academy Press. pp. 68–70. ISBN 978-0-309-05230-6.
- ^ "Intended and Unintended Births in the United States: 1982–2010" (PDF). Centers for Disease Control. 24 July 2012. Retrieved 3 September 2019.
- ^ Baliunas D, Rehm J, Irving H, Shuper P (June 2010). "Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis". International Journal of Public Health. 55 (3): 159–166. doi:10.1007/s00038-009-0095-x. PMID 19949966.
- ^ Fisher JC, Bang H, Kapiga SH (November 2007). "The association between HIV infection and alcohol use: a systematic review and meta-analysis of African studies". Sexually Transmitted Diseases. 34 (11): 856–863. doi:10.1097/OLQ.0b013e318067b4fd. PMID 18049422.
- ^ Kabapy AF, Shatat HZ, Abd El-Wahab EW (November 2020). "Attributes of HIV infection over decades (1982-2018): A systematic review and meta-analysis". Transboundary and Emerging Diseases. 67 (6): 2372–2388. doi:10.1111/tbed.13621. PMID 32396689.
- ^ a b c Rehm J, Probst C, Shield KD, Shuper PA (February 2017). "Does alcohol use have a causal effect on HIV incidence and disease progression? A review of the literature and a modeling strategy for quantifying the effect". Population Health Metrics. 15 (1): 4. doi:10.1186/s12963-017-0121-9. PMC 5301358. PMID 28183309.
- ^ a b Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J (2010). "Causal considerations on alcohol and HIV/AIDS--a systematic review". Alcohol and Alcoholism. 45 (2). Oxford, Oxfordshire: 159–66. doi:10.1093/alcalc/agp091. PMID 20061510.
- ^ Manthey J, Hassan SA, Carr S, Kilian C, Kuitunen-Paul S, Rehm J (July 2021). "What are the Economic Costs to Society Attributable to Alcohol Use? A Systematic Review and Modelling Study". PharmacoEconomics. 39 (7): 809–822. doi:10.1007/s40273-021-01031-8. PMC 8200347. PMID 33970445.
- ^ Lee GA, Forsythe M (July 2011). "Is alcohol more dangerous than heroin? The physical, social and financial costs of alcohol". International Emergency Nursing. 19 (3): 141–145. doi:10.1016/j.ienj.2011.02.002. PMID 21665157.
- ^ Cheng B, Lim CC, Rutherford BN, Huang S, Ashley DP, Johnson B, et al. (January 2024). "A systematic review and meta-analysis of the relationship between youth drinking, self-posting of alcohol use and other social media engagement (2012–21)". Addiction. 119 (1): 28–46. doi:10.1111/add.16304. PMID 37751678.
- ^ Virtanen M, Jokela M, Nyberg ST, Madsen IE, Lallukka T, Ahola K, et al. (January 2015). "Long working hours and alcohol use: systematic review and meta-analysis of published studies and unpublished individual participant data". BMJ. 350: g7772. doi:10.1136/bmj.g7772. PMC 4293546. PMID 25587065.
- ^ Amiri S (April 2022). "Smoking and alcohol use in unemployed populations: a systematic review and meta-analysis". Journal of Addictive Diseases. 40 (2): 254–277. doi:10.1080/10550887.2021.1981124. PMID 34747337.
- ^ Borsari B, Murphy JG, Barnett NP (October 2007). "Predictors of alcohol use during the first year of college: implications for prevention". Addictive Behaviors. 32 (10): 2062–2086. doi:10.1016/j.addbeh.2007.01.017. PMC 2614076. PMID 17321059.
- ^ Steinfatt TM (2002). Working at the Bar: Sex Work and Health Communication in Thailand. Greenwood Publishing Group. p. 35. ISBN 9781567505672.
- ^ Kishindo P (1995). "Sexual behaviour in the face of risk: the case of bar girls in Malawi's major cities". Health Transition Review. 5 (Supplement: The Third World AIDS Epidemic). National Center for Epidemiology and Population Health (NCEPH), The Australian National University: 153–160. JSTOR 40652159.
- ^ Bell D, Hadjiefthyvoulou F (August 2022). "Alcohol and drug use among bartenders: An at risk population?". Journal of Substance Abuse Treatment. 139: 108762. doi:10.1016/j.jsat.2022.108762. PMID 35361512.
- ^ Muniz K (24 March 2014). "20 ways Americans are blowing their money". USA Today. Retrieved 16 October 2018.
- ^ Hanson-Easey S, Every D, Tehan B, Richardson J, Krackowizer A (2016). "Climate change, housing and homelessness: Report on the homelessness and climate change forum (why are climate change and homelessness in the same category?)" (PDF). Archived from the original (PDF) on 14 April 2019. Retrieved 18 March 2019.
- ^ Pascale CM (1 May 2005). "There's No Place Like Home: The Discursive Creation of Homelessness". Cultural Studies ↔ Critical Methodologies. 5 (2): 250–268. doi:10.1177/1532708605274558. S2CID 143284882.
- ^ Osborn A (June 2005). "Russia's youth faces worst crisis of homelessness and substance misuse since second world war". BMJ. 330 (7504): 1348. doi:10.1136/bmj.330.7504.1348-b. PMC 558316. PMID 15947386.
- ^ Embleton L, Mwangi A, Vreeman R, Ayuku D, Braitstein P (October 2013). "The epidemiology of substance use among street children in resource-constrained settings: a systematic review and meta-analysis". Addiction. 108 (10). Abingdon, England: 1722–1733. doi:10.1111/add.12252. PMC 3776018. PMID 23844822.
- ^ "Holidaymakers warned over alcohol ban in Ibiza and Majorca". The Independent. 11 May 2024.
- ^ Youssef NA, Rich CL (2008). "Does acute treatment with sedatives/hypnotics for anxiety in depressed patients affect suicide risk? A literature review". Annals of Clinical Psychiatry. 20 (3): 157–169. doi:10.1080/10401230802177698. PMID 18633742.
- ^ a b Vijayakumar L, Kumar MS, Vijayakumar V (May 2011). "Substance use and suicide". Current Opinion in Psychiatry. 24 (3): 197–202. doi:10.1097/YCO.0b013e3283459242. PMID 21430536. S2CID 206143129.
- ^ a b Sher L (January 2006). "Alcohol consumption and suicide". QJM. 99 (1): 57–61. doi:10.1093/qjmed/hci146. PMID 16287907.
- ^ Sher L (2007). "Functional magnetic resonance imaging in studies of the neurobiology of suicidal behavior in adolescents with alcohol use disorders". International Journal of Adolescent Medicine and Health. 19 (1): 11–18. doi:10.1515/ijamh.2007.19.1.11. PMID 17458319. S2CID 42672912.
- ^ Wei B, Liu Y, Li H, Peng Y, Luo Z (February 2023). "Impact of alcohol consumption on coronavirus disease 2019 severity: A systematic review and meta-analysis". Journal of Medical Virology. 95 (2): e28547. doi:10.1002/jmv.28547. PMID 36734064.
- ^ Park SH, Kim DJ (October 2020). "Global and regional impacts of alcohol use on public health: Emphasis on alcohol policies". Clinical and Molecular Hepatology. 26 (4): 652–661. doi:10.3350/cmh.2020.0160. PMC 7641561. PMID 33053937.
- ^ Iida-Ueno A, Enomoto M, Tamori A, Kawada N (April 2017). "Hepatitis B virus infection and alcohol consumption". World Journal of Gastroenterology. 23 (15): 2651–2659. doi:10.3748/wjg.v23.i15.2651. PMC 5403744. PMID 28487602.
- ^ Maintz L, Novak N (May 2007). "Histamine and histamine intolerance". The American Journal of Clinical Nutrition. 85 (5): 1185–1196. doi:10.1093/ajcn/85.5.1185. PMID 17490952.
- ^ Kushner MG, Abrams K, Borchardt C (March 2000). "The relationship between anxiety disorders and alcohol use disorders: a review of major perspectives and findings". Clinical Psychology Review. 20 (2): 149–171. doi:10.1016/s0272-7358(99)00027-6. PMID 10721495.
- ^ Castillo-Carniglia A, Keyes KM, Hasin DS, Cerdá M (December 2019). "Psychiatric comorbidities in alcohol use disorder". The Lancet. Psychiatry. 6 (12): 1068–1080. doi:10.1016/S2215-0366(19)30222-6. PMC 7006178. PMID 31630984.
- ^ Kessler RC (November 2004). "The epidemiology of dual diagnosis". Biological Psychiatry. 56 (10): 730–737. doi:10.1016/j.biopsych.2004.06.034. PMID 15556117.
- ^ Puddephatt JA, Irizar P, Jones A, Gage SH, Goodwin L (June 2022). "Associations of common mental disorder with alcohol use in the adult general population: a systematic review and meta-analysis". Addiction. 117 (6): 1543–1572. doi:10.1111/add.15735. PMC 9300028. PMID 34729837.
- ^ Greydanus DE, Shek D (September 2009). "Deliberate self-harm and suicide in adolescents". The Keio Journal of Medicine. 58 (3): 144–151. doi:10.2302/kjm.58.144. hdl:10397/4495. PMID 19826208.
- ^ Bolton J, Cox B, Clara I, Sareen J (November 2006). "Use of alcohol and drugs to self-medicate anxiety disorders in a nationally representative sample". The Journal of Nervous and Mental Disease. 194 (11): 818–825. doi:10.1097/01.nmd.0000244481.63148.98. PMID 17102705. S2CID 7515999.
- ^ Peters GL, Rosselli JL, Kerr JL. "Overview of Peptic Ulcer Disease: Etiology and Pathophysiology". Medscape.com. Retrieved 27 April 2013.
- ^ D'Souza S, Mayock S, Salt A (December 2017). "A review of in vivo and in vitro aspects of alcohol-induced dose dumping". AAPS Open. 3 (1). doi:10.1186/s41120-017-0014-9. ISSN 2364-9534.
- ^ a b c Yost DA (2002). "Acute care for alcohol intoxication" (PDF). Postgraduate Medicine Online. 112 (6). Archived from the original (PDF) on 14 December 2010. Retrieved 29 September 2007.
- ^ Lukas SE, Orozco S (October 2001). "Ethanol increases plasma Delta(9)-tetrahydrocannabinol (THC) levels and subjective effects after marihuana smoking in human volunteers". Drug and Alcohol Dependence. 64 (2): 143–9. doi:10.1016/S0376-8716(01)00118-1. PMID 11543984.
- ^ TOMSO entry in PiHKAL
- ^ "Harmful Interactions | National Institute on Alcohol Abuse and Alcoholism (NIAAA)". www.niaaa.nih.gov.
- ^ Repchinsky C (ed.) (2012). Compendium of pharmaceuticals and specialties, Ottawa: Canadian Pharmacists Association.[full citation needed]
- ^ "Alcohol & Diabetes – ADA". American Diabetes Association. Retrieved 30 November 2022.
- ^ Agrawal N (June 1991). "Risk factors for gastrointestinal ulcers caused by nonsteroidal anti-inflammatory drugs (NSAIDs)". The Journal of Family Practice. 32 (6): 619–624. PMID 2040888.
- ^ "Aspirin information from Drugs.com". Drugs.com. Archived from the original on 9 May 2008. Retrieved 8 May 2008.
- ^ "Oral Aspirin information". First DataBank. Archived from the original on 18 September 2000. Retrieved 8 May 2008.
- ^ Curran CP, Marczinski CA (December 2017). "Taurine, caffeine, and energy drinks: Reviewing the risks to the adolescent brain". Birth Defects Research. 109 (20): 1640–1648. doi:10.1002/bdr2.1177. PMC 5737830. PMID 29251842.
- ^ Arria AM, Caldeira KM, Kasperski SJ, O'Grady KE, Vincent KB, Griffiths RR, et al. (June 2010). "Increased alcohol consumption, nonmedical prescription drug use, and illicit drug use are associated with energy drink consumption among college students". Journal of Addiction Medicine. 4 (2): 74–80. doi:10.1097/ADM.0b013e3181aa8dd4. PMC 2923814. PMID 20729975.
- ^ "Energy drinks and risk to future substance use". www.drugabuse.gov. National Institute on Drug Abuse. 8 August 2017. Archived from the original on 18 February 2020. Retrieved 29 March 2019.
- ^ Laizure SC, Mandrell T, Gades NM, Parker RB (January 2003). "Cocaethylene metabolism and interaction with cocaine and ethanol: role of carboxylesterases". Drug Metabolism and Disposition. 31 (1): 16–20. doi:10.1124/dmd.31.1.16. PMID 12485948.
- ^ Pergolizzi J, Breve F, Magnusson P, LeQuang JA, Varrassi G (February 2022). "Cocaethylene: When Cocaine and Alcohol Are Taken Together". Cureus. 14 (2): e22498. doi:10.7759/cureus.22498. PMC 8956485. PMID 35345678.
- ^ Markowitz JS, Logan BK, Diamond F, Patrick KS (August 1999). "Detection of the novel metabolite ethylphenidate after methylphenidate overdose with alcohol coingestion". Journal of Clinical Psychopharmacology. 19 (4): 362–6. doi:10.1097/00004714-199908000-00013. PMID 10440465.
- ^ Markowitz JS, DeVane CL, Boulton DW, Nahas Z, Risch SC, Diamond F, et al. (June 2000). "Ethylphenidate formation in human subjects after the administration of a single dose of methylphenidate and ethanol". Drug Metabolism and Disposition. 28 (6): 620–4. PMID 10820132.
- ^ Verplaetse TL, McKee SA (March 2017). "An overview of alcohol and tobacco/nicotine interactions in the human laboratory". The American Journal of Drug and Alcohol Abuse. 43 (2): 186–196. doi:10.1080/00952990.2016.1189927. PMC 5588903. PMID 27439453.
- ^ McCoy HG, Cipolle RJ, Ehlers SM, Sawchuk RJ, Zaske DE (November 1979). "Severe methanol poisoning. Application of a pharmacokinetic model for ethanol therapy and hemodialysis". The American Journal of Medicine. 67 (5): 804–7. doi:10.1016/0002-9343(79)90766-6. PMID 507092.
- ^ Weathermon R, Crabb DW (1999). "Alcohol and medication interactions". Alcohol Research & Health. 23 (1): 40–54. PMC 6761694. PMID 10890797.
- ^ "PRODUCT INFORMATION COUMADIN" (PDF). TGA eBusiness Services. Aspen Pharma Pty Ltd. 19 January 2010. Archived from the original on 17 October 2015. Retrieved 11 December 2013.
- ^ "Warfarin Anticoagulant Medication". Archived from the original on 1 July 2020. Retrieved 30 June 2020.
- ^ "Isoniazid tablet". DailyMed. 18 October 2018. Archived from the original on 13 March 2019. Retrieved 24 January 2020.
- ^ Saukkonen JJ, Cohn DL, Jasmer RM, Schenker S, Jereb JA, Nolan CM, et al. (October 2006). "An official ATS statement: hepatotoxicity of antituberculosis therapy". American Journal of Respiratory and Critical Care Medicine. 174 (8): 935–952. doi:10.1164/rccm.200510-1666ST. PMID 17021358. S2CID 36384722.
- ^ a b Lobo IA, Harris RA (July 2008). "GABA(A) receptors and alcohol". Pharmacology Biochemistry and Behavior. 90 (1): 90–94. doi:10.1016/j.pbb.2008.03.006. PMC 2574824. PMID 18423561.
- ^ "Acetate, Ion chromatography standard solution, Safety Data Sheet". Thermo Fisher Scientific. 1 April 2024. p. 4.
- ^ Maxwell CR, Spangenberg RJ, Hoek JB, Silberstein SD, Oshinsky ML (December 2010). "Acetate causes alcohol hangover headache in rats". PLOS ONE. 5 (12): e15963. Bibcode:2010PLoSO...515963M. doi:10.1371/journal.pone.0015963. PMC 3013144. PMID 21209842.
- ^ 'Is coffee the real cure for a hangover?' by Bob Holmes, New Scientist, Jan. 15 2011, p. 17.
- ^ Narahashi T, Kuriyama K, Illes P, Wirkner K, Fischer W, Mühlberg K, et al. (May 2001). "Neuroreceptors and ion channels as targets of alcohol". Alcoholism: Clinical and Experimental Research. 25 (5 Suppl ISBRA): 182S–188S. doi:10.1097/00000374-200105051-00030. PMID 11391069.
- ^ Olsen RW, Li GD, Wallner M, Trudell JR, Bertaccini EJ, Lindahl E, et al. (March 2014). "Structural models of ligand-gated ion channels: sites of action for anesthetics and ethanol". Alcoholism: Clinical and Experimental Research. 38 (3): 595–603. doi:10.1111/acer.12283. PMC 3959612. PMID 24164436.
- ^ Charlet K, Beck A, Heinz A (2013). "The dopamine system in mediating alcohol effects in humans". Current Topics in Behavioral Neurosciences. 13: 461–88. doi:10.1007/7854_2011_130. ISBN 978-3-642-28719-0. PMID 21533679.
- ^ Méndez M, Morales-Mulia M (June 2008). "Role of mu and delta opioid receptors in alcohol drinking behaviour". Current Drug Abuse Reviews. 1 (2): 239–52. doi:10.2174/1874473710801020239. PMID 19630722.
- ^ Tillonen J. Ethanol, acetaldehyde and gastrointestinal flora (PDF) (Ph.D. thesis). Helsingin Yliopisto.
- ^ "Drunkest driver in SA arrested". SowetanLIVE. Retrieved 12 April 2024.
- ^ Zaridze D, Brennan P, Boreham J, Boroda A, Karpov R, Lazarev A, et al. (June 2009). "Alcohol and cause-specific mortality in Russia: a retrospective case-control study of 48,557 adult deaths". Lancet. 373 (9682): 2201–2214. doi:10.1016/S0140-6736(09)61034-5. PMC 2715218. PMID 19560602.
- ^ US Drug Enforcement Administration (May 2003). "Speaking Out Against Drug Legalization" (PDF). U.S. Department of Justice. Archived from the original (PDF) on 27 June 2006. Retrieved 21 October 2016.
- ^ Mokdad AH, Marks JS, Stroup DF, Gerberding JL (March 2004). "Actual causes of death in the United States, 2000" (PDF). JAMA. 291 (10): 1238–45. doi:10.1001/jama.291.10.1238. PMID 15010446. Archived from the original (PDF) on 17 September 2011.
- ^ NIAAA (August 2001). "Number of deaths and age-adjusted death rates per 100,000 population for categories of alcohol-related (A-R) mortality, United States and States, 1979–96". Database Resources / Statistical Tables. National Institute on Alcohol Abuse and Alcoholism (NIAAA). Archived from the original on 7 August 2007. Retrieved 20 October 2007.
- ^ Guillén-Mancina E, Calderón-Montaño JM, López-Lázaro M (February 2018). "Avoiding the ingestion of cytotoxic concentrations of ethanol may reduce the risk of cancer associated with alcohol consumption". Drug and Alcohol Dependence. 183: 201–204. doi:10.1016/j.drugalcdep.2017.11.013. PMID 29289868.
- ^ Lieber CS (1990). "Mechanism of ethanol induced hepatic injury". Pharmacology & Therapeutics. 46 (1): 1–41. doi:10.1016/0163-7258(90)90032-w. PMID 2181486.
- ^ Brust JC (April 2010). "Ethanol and cognition: indirect effects, neurotoxicity and neuroprotection: a review". International Journal of Environmental Research and Public Health. 7 (4): 1540–57. doi:10.3390/ijerph7041540. PMC 2872345. PMID 20617045.
- ^ "Hornets can hold their alcohol like no other animal on Earth". New Scientist.
- ^ "Distillation: Some Purity Considerations". Moonshine Still. Retrieved 5 May 2015.
- ^ Blumenthal P, Steger MC, Einfalt D, Rieke-Zapp J, Quintanilla Bellucci A, Sommerfeld K, et al. (April 2021). "Methanol Mitigation during Manufacturing of Fruit Spirits with Special Consideration of Novel Coffee Cherry Spirits". Molecules. 26 (9): 2585. doi:10.3390/molecules26092585. PMC 8125215. PMID 33925245.
- ^ Ma HL, Yang XP, Zuo Y (15 April 2006). "Study on Method of Decreasing Methanol in Apple Pomace Spirit". Food Science. 27 (4): 138–142.
- ^ Clark J, Farmer S, Kennepohl D, Kabrhel J, Ashenhurst J, Ashenhurst J (26 August 2015). "17.7: Oxidation of Alcohols". Chemistry LibreTexts.
- ^ Burcham PC (19 November 2013). An Introduction to Toxicology. Springer Science & Business Media. pp. 42–. ISBN 978-1-4471-5553-9.
- ^ Janssen MM, Mathijssen JJ, van Bon-Martens MJ, van Oers HA, Garretsen HF (June 2013). "Effectiveness of alcohol prevention interventions based on the principles of social marketing: a systematic review". Substance Abuse Treatment, Prevention, and Policy. 8 (1): 18. doi:10.1186/1747-597X-8-18. PMC 3679782. PMID 23725406.
- ^ World Health Organization (2014). "Global status report on alcohol and health 2014" (PDF). www.who.int. Retrieved 17 April 2015.
- ^ "Redefine alcohol: WHO's urgent call for Europe to rethink alcohol's place in society". www.who.int.
- ^ "What Is Intermittent Sobriety—and Why Is Everyone Talking About It Right Now?". Real Simple.
- ^ "Are You Trying 'Sober October'? Experts Reveal the Surprising Benefits of 'Intermittent Sobriety'". Health.
- ^ Goddiksen MK (4 January 2023). "Sober Curious er det nye sort'" [Sober Curious is the new kind] (in Danish).
- ^ "What Does It Mean to Be Sober Curious?". Henry Ford Health. 21 March 2023.
- ^ Boesen EG (February 2023). "Skål – uden alkohol". Samvirke (in Danish). pp. 18–27. ISSN 0036-3944.
- ^ Kilian C, O'Donnell A, Potapova N, López-Pelayo H, Schulte B, Miquel L, et al. (May 2022). "Changes in alcohol use during the COVID-19 pandemic in Europe: A meta-analysis of observational studies". Drug and Alcohol Review. 41 (4): 918–931. doi:10.1111/dar.13446. PMC 9111882. PMID 35187739.
- ^ "What We Eat in America, NHANES 2013–2014" (PDF). Archived (PDF) from the original on 24 February 2017. Retrieved 29 September 2021.
- ^ Zhao J, Stockwell T, Naimi T, Churchill S, Clay J, Sherk A (March 2023). "Association Between Daily Alcohol Intake and Risk of All-Cause Mortality: A Systematic Review and Meta-analyses". JAMA Network Open. 6 (3): e236185. doi:10.1001/jamanetworkopen.2023.6185. PMC 10066463. PMID 37000449.
- ^ Carr T, Kilian C, Llamosas-Falcón L, Zhu Y, Lasserre AM, Puka K, et al. (March 2024). "The risk relationships between alcohol consumption, alcohol use disorder and alcohol use disorder mortality: A systematic review and meta-analysis". Addiction. 119 (preprint): 1174–1187. doi:10.1111/add.16456. PMC 11156554. PMID 38450868.
- ^ Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, et al. (2010). Alcohol: No Ordinary Commodity: Research and Public Policy (2nd ed.). Oxford: Oxford University Press. ISBN 978-0-19-955114-9. OCLC 656362316.
- ^ Pinquart M (January 2024). "Change in Alcohol Consumption in Adolescence and Emerging Adulthood: A Meta-Analysis". Journal of Studies on Alcohol and Drugs. 85 (1): 41–50. doi:10.15288/jsad.22-00370. PMID 37650841.
- ^ a b Dunbar RI, Launay J, Wlodarski R, Robertson C, Pearce E, Carney J, et al. (June 2017). "Functional Benefits of (Modest) Alcohol Consumption". Adaptive Human Behavior and Physiology. 3 (2): 118–33. doi:10.1007/s40750-016-0058-4. PMC 7010365. PMID 32104646.
- ^ Sayette MA, Creswell KG, Dimoff JD, Fairbairn CE, Cohn JF, Heckman BW, et al. (August 2012). "Alcohol and group formation: a multimodal investigation of the effects of alcohol on emotion and social bonding". Psychological Science. 23 (8): 869–78. doi:10.1177/0956797611435134. PMC 5462438. PMID 22760882.
- ^ "Cheers or tears? WHO playbook exposes alcohol's true cost to health". www.who.int.
- ^ Druffner N, Egan D, Ramamurthy S, O'Brien J, Davis AF, Jack J, et al. (May 2024). "IQ in high school as a predictor of midlife alcohol drinking patterns". Alcohol and Alcoholism. 59 (4). doi:10.1093/alcalc/agae035. PMID 38804536.
- ^ "Higher IQ in High School Linked to Increased Alcohol Use in Adulthood". Neuroscience News. 11 October 2024.
- ^ Ruthven M (1997). Islam: a very short introduction. New York: Oxford University Press. ISBN 978-0-19-154011-0. OCLC 43476241.
- ^ "7b". Megillah (Talmud).
Rava said: A person is obligated to become intoxicated with wine on Purim until he is so intoxicated that he does not know how to distinguish between cursed is Haman and blessed is Mordecai.
- ^ Borras L, Khazaal Y, Khan R, Mohr S, Kaufmann YA, Zullino D, et al. (December 2010). "The relationship between addiction and religion and its possible implication for care". Substance Use & Misuse. 45 (14): 2357–2410. doi:10.3109/10826081003747611. PMC 4137975. PMID 21039108.
- ^ "Drinking on Purim". aishcom. 28 February 2015.
- ^ Zanders ED (2011). "Introduction to Drugs and Drug Targets". The Science and Business of Drug Discovery. Springer. pp. 11–27. doi:10.1007/978-1-4419-9902-3_2. ISBN 978-1-4419-9901-6. PMC 7120710.
- ^ Room R (2007). "National Variations in the use of Alcohol and Drug Research: Notes of an itinerant worker". Nordic Studies on Alcohol and Drugs. 24 (6): 634–640. doi:10.1177/145507250702400611. ISSN 1455-0725.
- ^ Farrell M (2007). "The alcohol industry: Taking on the public health critics". British Medical Journal. 335 (7621): 671. doi:10.1136/bmj.39337.431667.4E. PMC 1995479.
- ^ WHO | Lexicon of alcohol and drug terms published by the World Health Organization. Who.int (2010-12-09). Retrieved on 2011-09-24.
- ^ Sienkiewicz P (2011). "[Ethyl alcohol and psychoactive drugs in patients with head and trunk injuries treated at the Department of General Surgery, Provincial Hospital in Siedlce]". Annales Academiae Medicae Stetinensis. 57 (1): 96–104. PMID 22593998.
- ^ Odette MM, Porucznik CA, Gren LH, Garland EL (March 2024). "Alcohol consumption and opioid craving among chronic pain patients prescribed long-term opioid therapy". Addictive Behaviors. 150: 107911. doi:10.1016/j.addbeh.2023.107911. PMC 11257353. PMID 38039857.
- ^ Sznitman SR, Kolobov T, Bogt TT, Kuntsche E, Walsh SD, Boniel-Nissim M, et al. (November 2013). "Exploring substance use normalization among adolescents: a multilevel study in 35 countries". Social Science & Medicine. 97: 143–151. doi:10.1016/j.socscimed.2013.08.038. PMID 24161099.
- ^ Sellman D, Connor J, Robinson G, Jackson R (September 2009). "Alcohol cardio-protection has been talked up". The New Zealand Medical Journal. 122 (1303): 97–101. PMID 19851424.
- ^ a b c d e Boyle P (7 March 2013). Alcohol: Science, Policy and Public Health. OUP Oxford. pp. 363–. ISBN 978-0-19-965578-6.
- ^ "Getting a drink in Saudi Arabia". BBC News. BBC. 8 February 2001. Retrieved 7 July 2015.
- ^ "Can you drink alcohol in Saudi Arabia?". 1 August 2012. Retrieved 7 July 2015.
- ^ "13 Countries With Booze Bans". Swifty.com. Archived from the original on 2 July 2015. Retrieved 7 July 2015.
- ^ "Two Iranians Sentenced to Death for Drinking Alcohol, AFP Says – Businessweek". Archived from the original on 28 June 2012. Retrieved 25 June 2012.
- ^ "Iran to execute two for alcohol: Reports". Archived from the original on 25 June 2012. Retrieved 25 June 2012.
- ^ Zhao J, Stockwell T, Vallance K, Hobin E (March 2020). "The Effects of Alcohol Warning Labels on Population Alcohol Consumption: An Interrupted Time Series Analysis of Alcohol Sales in Yukon, Canada". Journal of Studies on Alcohol and Drugs. 81 (2): 225–37. doi:10.15288/jsad.2020.81.225. PMID 32359054. S2CID 218481829.
- ^ "Alcohol labelling: A discussion document on policy options" (PDF). World Health Organization. Archived from the original (PDF) on 18 August 2022. Retrieved 22 March 2024.
- ^ "Minimum alcohol unit price in Scotland to rise to 65p". 8 February 2024.
- ^ a b "2019 AICR Cancer Risk Awareness Survey" (PDF). AICR 2019 Cancer Risk Awareness Survey. 2019.
- ^ Greene NK, Rising CJ, Seidenberg AB, Eck R, Trivedi N, Oh AY (May 2023). "Exploring correlates of support for restricting breast cancer awareness marketing on alcohol containers among women". The International Journal on Drug Policy. 115: 104016. doi:10.1016/j.drugpo.2023.104016. PMC 10593197. PMID 36990013.
- ^ Atkinson AM, Meadows BR, Sumnall H (February 2024). "'Just a colour?': Exploring women's relationship with pink alcohol brand marketing within their feminine identity making". The International Journal on Drug Policy. 125: 104337. doi:10.1016/j.drugpo.2024.104337. PMID 38335868.
- ^ Hall MG, Lee CJ, Jernigan DH, Ruggles P, Cox M, Whitesell C, et al. (May 2024). "The impact of "pinkwashed" alcohol advertisements on attitudes and beliefs: A randomized experiment with US adults". Addictive Behaviors. 152: 107960. doi:10.1016/j.addbeh.2024.107960. PMC 10923020. PMID 38309239.
- ^ Mart S, Giesbrecht N (October 2015). "Red flags on pinkwashed drinks: contradictions and dangers in marketing alcohol to prevent cancer". Addiction. 110 (10): 1541–1548. doi:10.1111/add.13035. PMID 26350708.
- ^ Spivey JD, Lee JG, Smallwood SW (February 2018). "Tobacco Policies and Alcohol Sponsorship at Lesbian, Gay, Bisexual, and Transgender Pride Festivals: Time for Intervention". American Journal of Public Health. 108 (2): 187–188. doi:10.2105/AJPH.2017.304205. PMC 5846596. PMID 29320286.
- ^ Adams J, Asiasiga L, Neville S (October 2023). "The alcohol industry-A commercial determinant of poor health for Rainbow communities". Health Promotion Journal of Australia. 34 (4): 903–909. doi:10.1002/hpja.665. PMID 36103136.
- ^ "AUDIT The Alcohol Use Disorders Identification Test" (pdf). WHO (2nd ed.). 2001. Retrieved 2 January 2020.
- ^ Kalinowski A, Humphreys K (July 2016). "Governmental standard drink definitions and low-risk alcohol consumption guidelines in 37 countries". Addiction. 111 (7): 1293–1298. doi:10.1111/add.13341. PMID 27073140.
- ^ Jones AW (1991). "Forensic Science Aspects of Ethanol Metabolism". Forensic Science Progress 5. Vol. 5. pp. 31–89. doi:10.1007/978-3-642-58233-2_2. ISBN 978-3-540-53203-3.
- ^ Jones AW (September 2019). "Alcohol, its absorption, distribution, metabolism, and excretion in the body and pharmacokinetic calculations". WIREs Forensic Science. 1 (5). doi:10.1002/wfs2.1340.
- ^ Eger II EI, Saidman LJ, Westhorpe RN (14 September 2013). The Wondrous Story of Anesthesia. Springer Science & Business Media. pp. 4–. ISBN 978-1-4614-8441-7. Archived from the original on 18 September 2017.
- ^ Shah JB (September 2011). "The history of wound care". The Journal of the American College of Certified Wound Specialists. 3 (3): 65–66. doi:10.1016/j.jcws.2012.04.002. PMC 3601883. PMID 24525756.
- ^ John Gill's Exposition of the Bible Classic Bible Commentaries
- ^ "Dutch". Oxford English Dictionary (2nd ed.). Oxford University Press. 1989.
- ^ Byrne E (26 July 2013). "What is the origin of the phrase 'Dutch Courage'?". History Extra. Retrieved 26 December 2022.
- ^ Martin G. "Dutch courage". Phrases. UK. Retrieved 26 December 2022.
- ^ "History of Alcohol" (PDF). Archived from the original (PDF) on 21 August 2013. Retrieved 11 May 2015.
- ^ "Gin Act". Britannica Online Encyclopedia.
- ^ "Motbok" [Counter book]. Förvaltningshistorisk ordbok [Administrative history dictionary] (in Swedish). Retrieved 3 November 2022.
- ^ Arjakas K (8 November 2008). "Alkoholikeeldudest Eestis" [Alcohol bans in Estonia]. Postimees (in Estonian). Retrieved 27 March 2024.
- ^ "Marijuana Research Report:Is marijuana a gateway drug?". National Institute on Drug Abuse. July 2020. Retrieved 7 November 2020.
- ^ Kirby T, Barry AE (2012). "Alcohol as a gateway drug: A study of US 12th graders" (PDF). Journal of School Health. 82 (8): 371–9. doi:10.1111/j.1746-1561.2012.00712.x. PMID 22712674. Archived from the original (PDF) on 4 June 2016. Retrieved 26 May 2016.
Further reading
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans (1988). Alcohol Drinking. International Agency for Research on Cancer.
External links
- "ETOH Database Search". hazelden.org.
- The National Institute on Alcohol Abuse and Alcoholism maintains a database of alcohol-related health effects. ETOH Archival Database (1972–2003) Alcohol and Alcohol Problems Science Database.
- "Harmful Interactions | National Institute on Alcohol Abuse and Alcoholism (NIAAA)". www.niaaa.nih.gov.
- WHO fact sheet on alcohol
- ChEBI – biology related
- Kyoto Encyclopedia of Genes and Genomes signal transduction pathway: KEGG – human alcohol addiction




